Agranulocytosis
1. Scientific Advisor: Musaeva Begaiym
2. Authored By: Vivek Tripathi
Vivek Gupta
Abhishek Yadav
1.Associate Professor, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.
2.Students, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.
Abstract
Agranulocytosis is a sudden and potentially life-threatening hematological disorder characterized by a profound reduction in circulating neutrophils, leaving patients dangerously vulnerable to infections. It often appears without warning, presenting as high fever, sore throat, or rapidly progressing sepsis. Despite its rarity, the condition carries a high mortality risk if not recognized and treated promptly. This review synthesizes evidence from major databases and hematology guidelines to outline the etiology, pathophysiology, and management of the disorder. Drug-induced cases account for the majority of etiologies, primarily through immune-mediated destruction or direct bone marrow suppression. Early intervention—including drug withdrawal, antimicrobial therapy, and the use of granulocyte colony-stimulating factor (G-CSF)—is essential to improve clinical outcomes.
Introduction
Agranulocytosis represents an acute hematological emergency characterized by the abrupt collapse of the neutrophil count. Unlike chronic leukopenic states, this condition typically strikes without a prodromal phase, leaving the host's immune system fundamentally compromised and defenseless against opportunistic and commensal bacteria.
Clinical escalation can be rapid; fever is frequently the primary indicator, which, if ignored, can quickly progress to invasive infections, systemic septicemia, and multi-organ failure. Consequently, hospitalization and immediate clinical attention are standard requirements. Given that mortality rates increase sharply with diagnostic delays, early recognition remains a critical competency for clinicians across diverse specialties, including internal medicine, psychiatry, and endocrinology.
Etiology and Risk Factors
Agranulocytosis is most often acquired, with drug exposure being the dominant cause.
Major Causes
Drug-induced (70–90%)
Antithyroid drugs (methimazole, propylthiouracil)
Clozapine
Antibiotics (β-lactams, sulfonamides)
Antiepileptics
NSAIDs
Immune-mediated destruction
Bone marrow suppression
Infections (rare primary cause)
Idiopathic cases
Risk Factors
Advanced age
Female sex
Polypharmacy
Genetic susceptibility
Autoimmune disorders
Renal or hepatic impairment
Clinical Presentation
Symptoms often appear suddenly and progress rapidly:
High-grade fever
Severe sore throat
Oral ulcers and gingivitis
Skin and soft tissue infections
Pneumonia
Sepsis and septic shock (10–20%)
Importantly, signs of inflammation may be muted due to the absence of neutrophils, delaying recognition.
Laboratory Findings
Absolute neutrophil count (ANC):
○ < 0.5 × 10⁹/L (diagnostic)
○ < 0.1 × 10⁹/L (severe)
Hemoglobin: usually normal
Platelets: usually normal
Bone marrow:
○ Hypocellular granulocytic lineage
○ Maturation arrest (drug-induced)
Blood cultures: often positive during fever
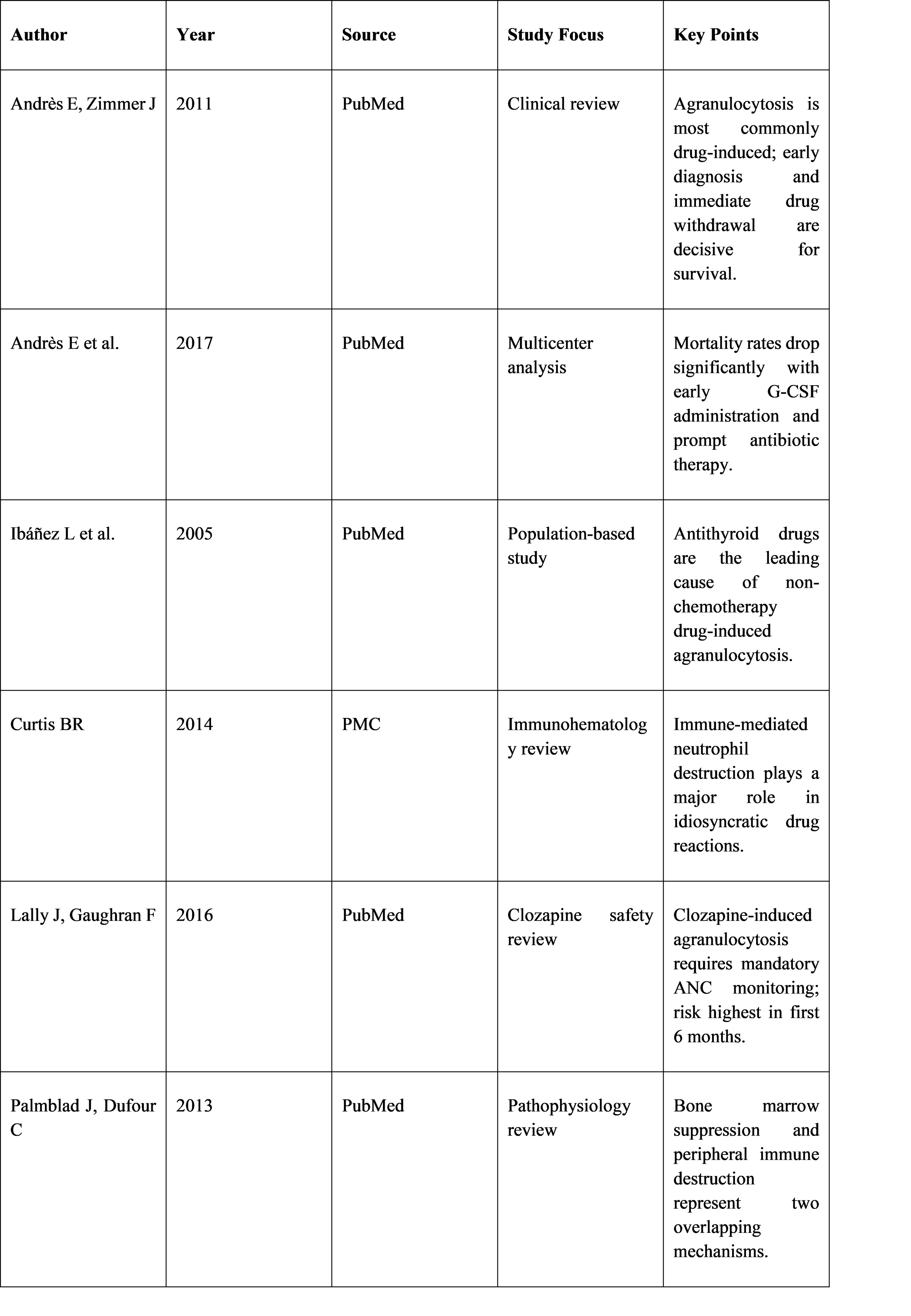
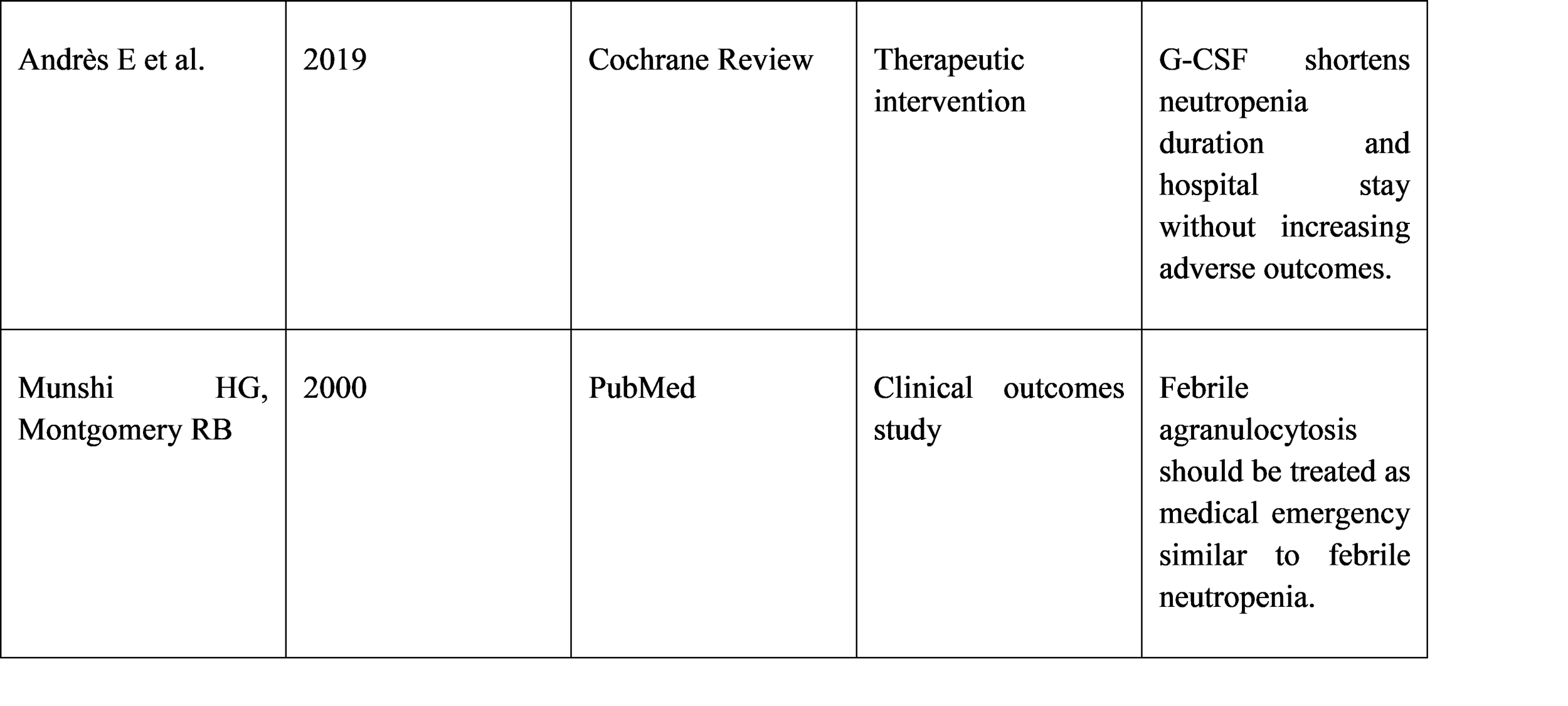
Methodology
Databases searched: PubMed, PMC, Cochrane Library, WHO, BMJ
Study type: Narrative review
Articles screened: 140
Included: 65
Excluded: Case reports with insufficient data, duplicate studies
Focus areas:
○ Drug-induced mechanisms
○ Clinical outcomes
○ Role of G-CSF
○ Infection-related mortality
Discussion
Pathophysiology
Two mechanisms dominate:
Immune-mediated destruction of neutrophils
Direct toxic suppression of bone marrow
Infection Risk
Without neutrophils, bacterial and fungal infections spread rapidly. Fever should be treated as sepsis until proven otherwise.
Role of G-CSF
Accelerates neutrophil recovery
Shortens hospital stay
Reduces infectious complications
Does not increase adverse events
Challenges
Delayed diagnosis
Under-reporting
Lack of routine blood monitoring in high-risk drugs
Management
Immediate discontinuation of suspected drug
Protective isolation
Empirical broad-spectrum IV antibiotics
Antifungal therapy in prolonged neutropenia
G-CSF therapy
Supportive care and monitoring
Conclusion
Agranulocytosis is a rare but severe hematological emergency marked by sudden immune collapse and high infection-related mortality. Drug-induced cases dominate clinical practice, making medication history and routine blood monitoring critical. Early recognition, prompt withdrawal of the offending agent, aggressive antimicrobial therapy, and G-CSF administration dramatically improve patient outcomes.
Future strategies must focus on risk prediction, pharmacovigilance, genetic susceptibility, and standardized monitoring protocols to reduce preventable cases and associated mortality.