Diabetes Insipidus in Children
1. Osmonova Gulnaz Zhenishbaevna
2. Nimmakuri Varun
(1. Teacher, Department of Pediatrics, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.
2. Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.)
Abstract
Diabetes insipidus (DI) in children is a rare endocrine disorder characterized by the excretion of large volumes of dilute urine due to impaired synthesis, secretion, or action of antidiuretic hormone (ADH). It may be congenital or acquired and, if untreated, can lead to severe dehydration, electrolyte imbalance, growth retardation, and neurological complications. This article reviews the etiopathogenesis, clinical manifestations, diagnostic criteria, differential diagnosis, treatment options, and long-term medical follow-up of diabetes insipidus in the pediatric population. Early recognition and appropriate management are essential to prevent morbidity and ensure normal growth and development.
Keywords: Diabetes insipidus, children, antidiuretic hormone, polyuria, polydipsia, central diabetes insipidus, nephrogenic diabetes insipidus
Introduction
Diabetes insipidus is a disorder of water metabolism caused by a deficiency of antidiuretic hormone or renal resistance to its effects. Unlike diabetes mellitus, it is not associated with hyperglycemia. In children, diabetes insipidus is particularly challenging due to nonspecific early symptoms and the limited ability of infants and young children to express thirst. The disease can be life-threatening if diagnosis is delayed. Pediatric DI is classified mainly into central diabetes insipidus (CDI) and nephrogenic diabetes insipidus (NDI), each with distinct etiologies and management approaches.
Objectives
1. To describe the etiopathogenesis of diabetes insipidus in children
2. To identify clinical manifestations across different pediatric age groups
3. To outline diagnostic criteria and investigations
4. To discuss differential diagnosis of polyuria and polydipsia
5. To summarize treatment strategies and principles of long-term medical follow-up
Methods
This review is based on a descriptive analysis of standard pediatric endocrinology textbooks, clinical guidelines, and peer-reviewed medical literature. Information was systematically collected regarding pathophysiology, clinical presentation, diagnostic tools, therapeutic approaches, and follow-up recommendations for diabetes insipidus in children.
Results
1.Etiopathogenesis
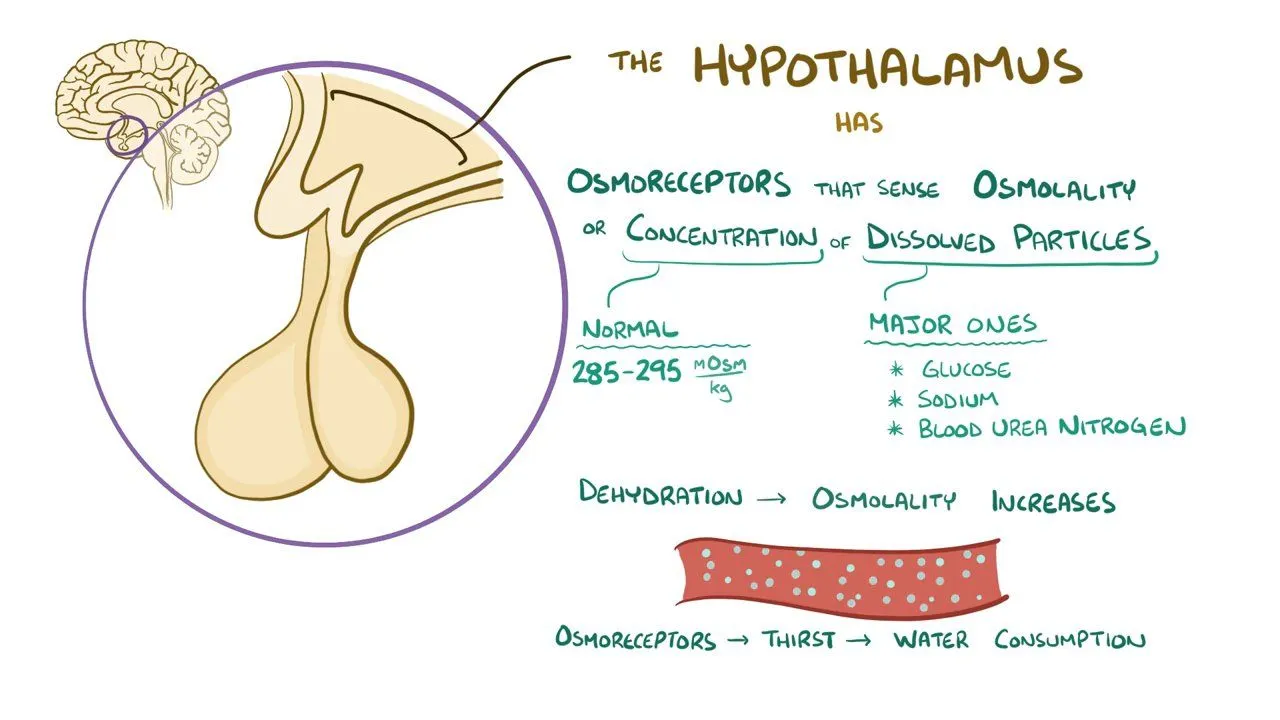
Diabetes insipidus occurs due to impaired ADH activity:
1. Central Diabetes Insipidus (CDI)
Caused by decreased synthesis or secretion of ADH from the hypothalamus or posterior pituitary.
Causes include:
• Congenital malformations
• Genetic mutations
• Brain tumors (craniopharyngioma, germinoma)
• Head trauma or neurosurgery
• Infections (meningitis, encephalitis)
• Idiopathic (most common in children)
2. Nephrogenic Diabetes Insipidus (NDI)
Caused by renal resistance to ADH.
Causes include:
• Congenital mutations (AVPR2 or AQP2 genes)
• Chronic kidney disease
• Electrolyte disturbances (hypercalcemia, hypokalemia)
• Drugs (e.g., lithium)
Clinical Features
Infants:
• Polyuria
• Poor weight gain
• Irritability
• Vomiting
• Fever of unknown origin
• Dehydration
Older children:
• Polyuria (large volumes of dilute urine)
• Polydipsia (preference for cold water)
• Nocturia and enuresis
• Fatigue
• Growth retardation
Diagnosis
• Detailed history (polyuria, polydipsia)
• Measurement of urine volume
• Low urine specific gravity (<1.005)
• Low urine osmolality
• Normal or high serum sodium and osmolality
• Water deprivation test (with caution in children
• Desmopressin (DDAVP) test to differentiate CDI from NDI
• MRI of brain and pituitary (for CDI)
Discussion
Diabetes insipidus in children requires a high index of suspicion due to its nonspecific presentation. Early diagnosis prevents severe dehydration and neurological damage. Differentiation between central and nephrogenic forms is essential for appropriate management. Advances in imaging and availability of desmopressin have significantly improved prognosis. However, long-term follow-up remains crucial to ensure normal growth, development, and quality of life.
References
1. Kliegman RM, et al. Nelson Textbook of Pediatrics. Elsevier.
2. Sperling MA. Pediatric Endocrinology. Saunders.
3. Lifshitz F. Pediatric Endocrinology. CRC Press.
4. UpToDate. Diabetes insipidus in children.
5. Melmed S, et al. Williams Textbook of Endocrinology. Elsevier.