Parathyroid Gland in Children
1. Osmonova Gulnaz Zhenishbaevna
2. Shifa
(1. Teacher, Dept. of Hospital Therapy, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
(2. Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
Abstract
Parathyroid gland disorders in children are uncommon but clinically significant due to their profound effects on calcium–phosphorus metabolism, bone development, neuromuscular function, and overall growth. This paper reviews hypoparathyroidism presenting with tetany, as well as primary and secondary hyperparathyroidism in the pediatric population. Emphasis is placed on etiopathogenesis, clinical manifestations, diagnostic approaches, differential diagnosis, treatment strategies, preventive measures, and long-term medical follow-up. Early recognition and appropriate management are essential to prevent irreversible complications such as skeletal deformities, nephrocalcinosis, and neurodevelopmental impairment.
Keywords: Parathyroid hormone, hypoparathyroidism, tetany, hyperparathyroidism, children, calcium metabolism, vitamin D, pediatrics
Introduction
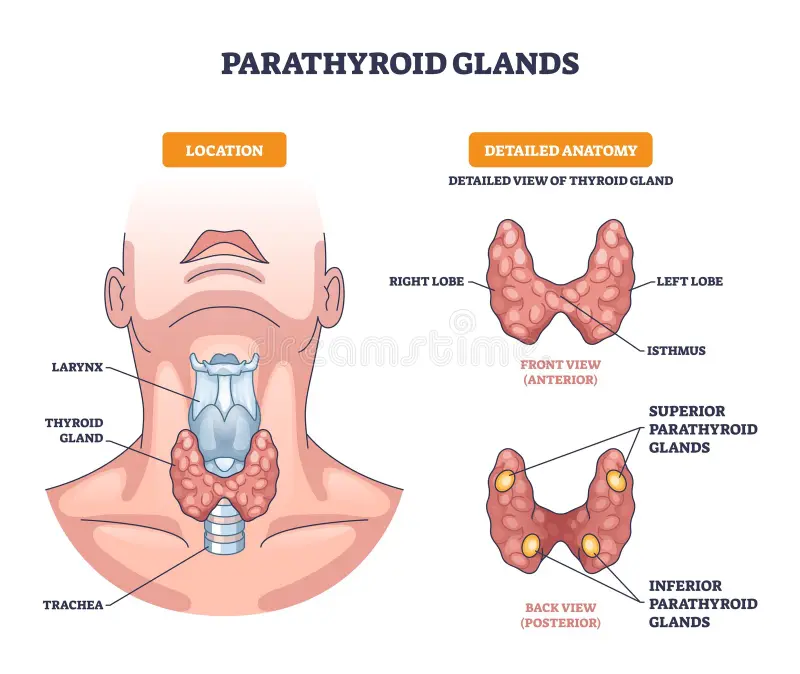
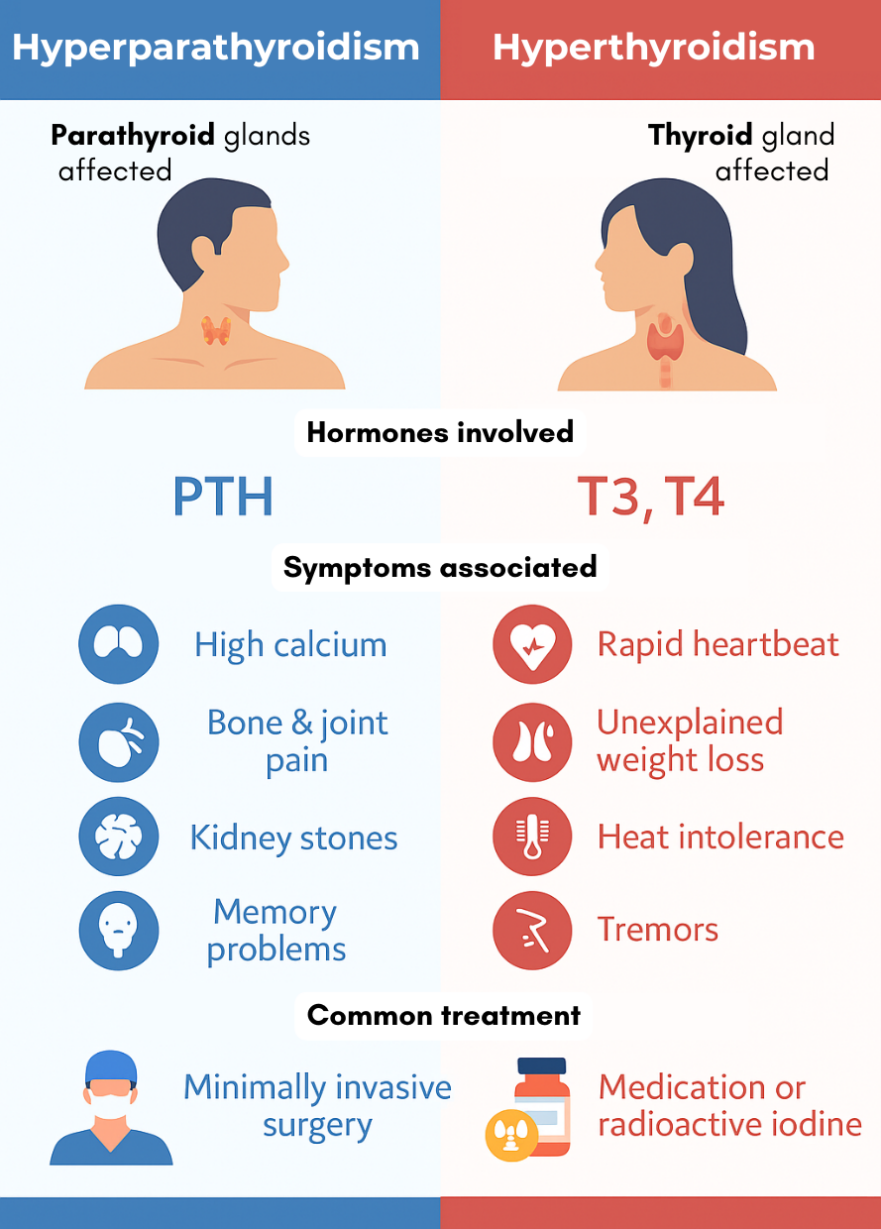
The parathyroid glands play a crucial role in maintaining calcium and phosphorus homeostasis through the secretion of parathyroid hormone (PTH). In children, disorders of parathyroid function disrupt skeletal mineralization, neuromuscular excitability, and metabolic balance. Although less frequent than in adults, pediatric parathyroid disorders often present with severe and acute symptoms. Hypoparathyroidism commonly manifests as hypocalcemic tetany, whereas hyperparathyroidism may be primary (due to intrinsic gland pathology) or secondary (most often due to chronic hypocalcemia or vitamin D deficiency). Understanding these conditions is vital for timely diagnosis and prevention of long-term morbidity.
Objectives
1. To describe the etiopathogenesis of hypoparathyroidism and hyperparathyroidism in children
2. To outline the clinical features of parathyroid gland disorders
3. To discuss diagnostic and differential diagnostic approaches
4. To review current treatment and prevention strategies
5. To highlight principles of long-term medical follow-up
Methods
This review is based on the analysis of standard pediatric endocrinology textbooks, clinical guidelines, and peer-reviewed articles focusing on calcium–phosphorus metabolism disorders in children. Data were synthesized to provide a structured overview following the IMRAD format.
Results
1. Etiopathogenesis
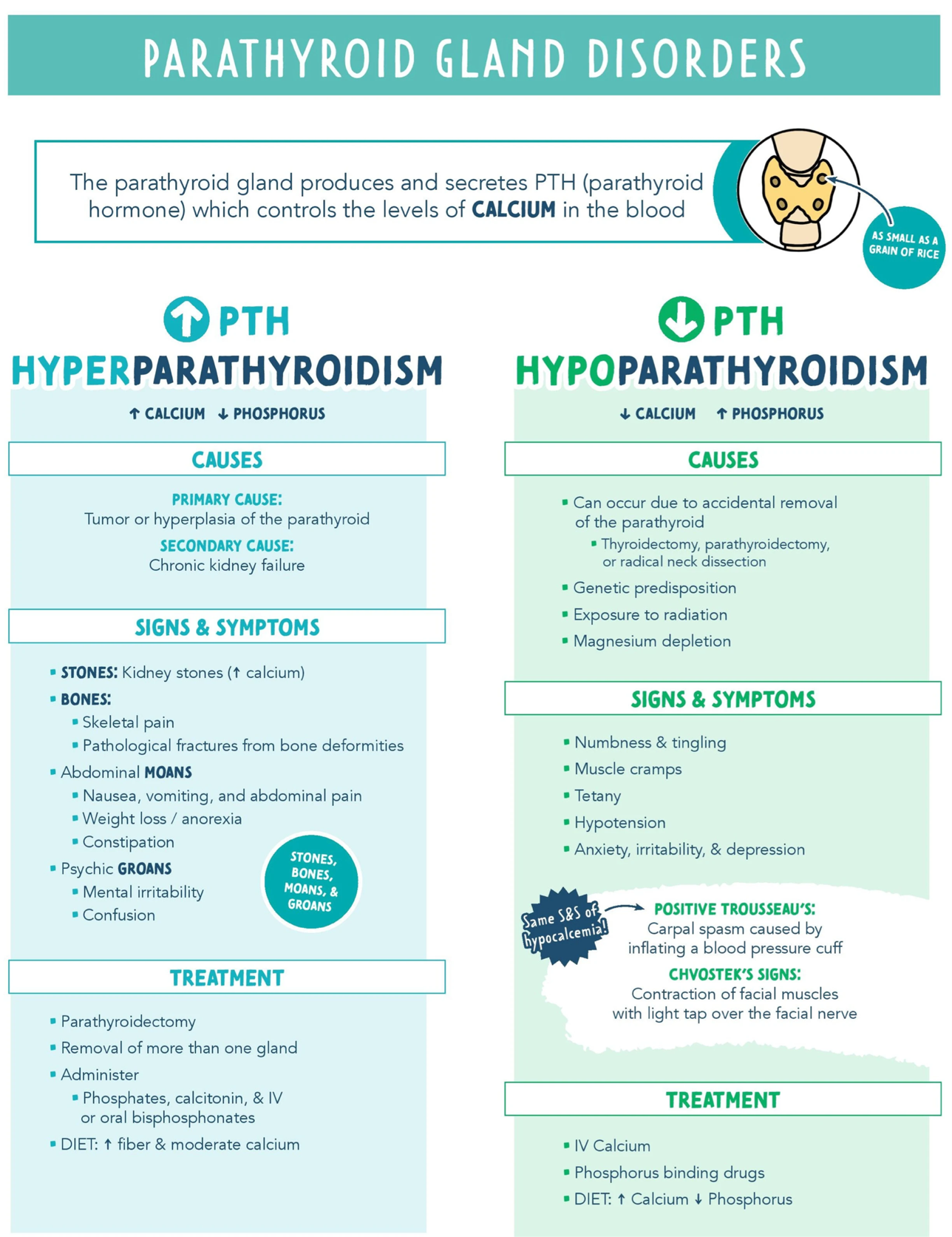
Hypoparathyroidism (Hypocalcemic Tetany)
• Congenital absence or hypoplasia of parathyroid glands (e.g., DiGeorge syndrome)
• Genetic defects in PTH synthesis or secretion
• Autoimmune destruction of parathyroid tissue
• Post-surgical damage or removal
• Functional hypoparathyroidism due to hypomagnesemia
Pathophysiology: ↓ PTH → ↓ serum calcium, ↑ serum phosphate → increased neuromuscular excitability
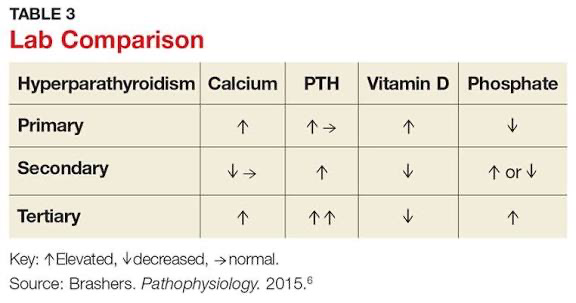
Primary Hyperparathyroidism
• Parathyroid adenoma (most common)
• Parathyroid hyperplasia
• Rare parathyroid carcinoma
• Genetic syndromes (MEN 1, MEN 2A)
Pathophysiology: Autonomous ↑ PTH secretion → hypercalcemia, bone resorption
Secondary Hyperparathyroidism
• Vitamin D deficiency or resistance
• Chronic kidney disease
• Malabsorption syndromes
• Nutritional rickets
Pathophysiology: Chronic hypocalcemia → compensatory ↑ PTH secretion
2. Clinical Manifestations
Hypoparathyroid Tetany
• Perioral numbness, paresthesia
• Muscle cramps, carpopedal spasm
• Laryngospasm, bronchospasm
• Seizures
• Positive Chvostek’s and Trousseau’s signs
Primary Hyperparathyroidism
• Bone pain, fractures
• Muscle weakness
• Polyuria, polydipsia
• Abdominal pain, constipation
• Nephrolithiasis (rare in children)
Secondary Hyperparathyroidism
• Signs of rickets or osteomalacia
• Bone deformities
• Growth retardation
• Muscle hypotonia
3. Diagnosis
• Laboratory tests:
• Serum calcium (↓ in hypoparathyroidism, ↑ in primary hyperparathyroidism)
• Serum phosphate (↑ in hypoparathyroidism)
• PTH levels
• Vitamin D levels
• Alkaline phosphatase (↑ in secondary hyperparathyroidism)
•Instrumental methods:
• X-ray of bones (rickets, osteopenia)
• Renal ultrasound (nephrocalcinosis, stones)
• Neck ultrasound or sestamibi scan (adenoma)
4. Differential Diagnosis
• Epilepsy (for tetany-related seizures)
• Hypocalcemia due to vitamin D deficiency
• Pseudohypoparathyroidism
• Renal tubular disorders
• Neuromuscular diseases
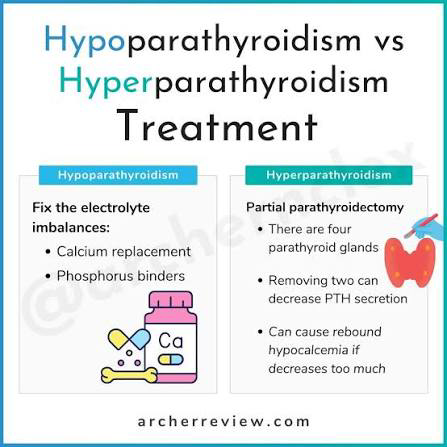
5. Treatment
Hypoparathyroidism
• Acute tetany: IV calcium gluconate
• Long-term: Oral calcium and active vitamin D (calcitriol)
• Correction of hypomagnesemia if present
Primary Hyperparathyroidism
• Surgical removal of adenoma or hyperplastic gland
• Medical management of hypercalcemia if surgery is delayed
Secondary Hyperparathyroidism
• Vitamin D supplementation
• Calcium supplementation
• Management of underlying renal or gastrointestinal disease
6. Prevention
• Adequate vitamin D and calcium intake
• Prevention of nutritional rickets
• Early treatment of chronic kidney disease
• Genetic counseling in hereditary cases
7. Medical Follow-Up
• Regular monitoring of serum calcium, phosphate, and PTH
• Growth and developmental assessment
• Renal function and ultrasound surveillance
• Adjustment of therapy to avoid hypercalcemia or nephrocalcinosis
Discussion
Parathyroid disorders in children present unique diagnostic and therapeutic challenges due to their rarity and overlap with other metabolic and neurological conditions. Hypoparathyroid tetany requires urgent recognition, while hyperparathyroidism often demands long-term etiological evaluation. Early diagnosis, targeted treatment, and continuous follow-up significantly improve outcomes and prevent complications affecting skeletal health and neurodevelopment.
References
1. Kliegman RM, St. Geme JW. Nelson Textbook of Pediatrics. Elsevier.
2. Sperling MA. Pediatric Endocrinology. Elsevier.
3. Jameson JL, Fauci AS. Harrison’s Principles of Internal Medicine.
4. European Society for Paediatric Endocrinology (ESPE) Clinical Guidelines.
5. Holick MF. Vitamin D deficiency. N Engl J Med.