Pediatric Endocrinology: Diseases of Thyroid Gland
1. Osmonova Gulnaaz Zh.
2. Muskan Kumawat
(1. Teacher, Department of Pediatrics, International Medical Faculty, Osh State University, Osh, Kyrgyzstan.
2. Medical Student, International Medical Faculty, Osh State University, Osh, Kyrgyzstan.)
ABSTRACT
Pediatric endocrinology is a specialist field that focuses on hormonal problems impacting growth, metabolism, and development in children and adolescents. The thyroid gland is one of the endocrine organs that is essential for controlling appropriate somatic growth, neurocognitive development, and metabolic activities. Endemic goiter, congenital hypothyroidism, and hyperthyroidism are examples of thyroid abnormalities, which are among the most prevalent endocrine issues in pediatric medicine. Iodine shortage is the main cause of endemic goiter, which results in compensatory thyroid enlargement from long-term TSH stimulation. If not identified early through prenatal screening, congenital hypothyroidism—which frequently results from thyroid dysgenesis or dyshormonogenesis—is a significant contributor to avoidable intellectual impairment. Children with hyperthyroidism, which is most frequently brought on by Graves' disease, have weight loss, tachycardia, and behavioral abnormalities as a result of autoimmune thyroid stimulation. To avoid irreparable developmental and cognitive problems, early detection, precise diagnosis utilizing biochemical and imaging techniques, and prompt therapeutic beginning are crucial. Public health initiatives, such as prenatal screening programs and universal salt iodization, continue to be essential parts of prevention. Thus, pediatric thyroid problems constitute a substantial clinical and public health issue, underscoring the significance of ongoing developments in pediatric endocrinology.
Keywords: Hormonal, Endocrine, Goiter, Tachycardia, Hypothyroidism, Prenatal, Dysgenesis, Biochemical, Iodine
INTRODUCTION
The diagnosis, treatment, and long-term management of hormonal abnormalities in newborns, children, and adolescents are the main objectives of pediatric endocrinology, a specialty area of medicine. Growth, metabolic balance, sexual development, and cognitively maturation are all significantly influenced by the endocrine system. Hormonal disruptions throughout childhood and adolescence can have serious, sometimes permanent effects since these are times of fast physical and neurological development. Therefore, to maintain normal growth trajectories, avoid developmental delays, and maximize long-term health outcomes, early detection and treatment of endocrine problems are crucial.
The thyroid hormones triiodothyronine (T3) and thyroxine (T4) are essential for somatic growth, brain development, thermoregulation, and metabolic control. Thyroid gland disorders are among the most prevalent endocrine issues that arise in pediatric medicine. These include endemic goiter, which is mostly linked to iodine shortage; congenital hypothyroidism, which, if left untreated, is a significant source of avoidable intellectual impairment; and pediatric hyperthyroidism, which is often brought on by the autoimmune disorder Graves' disease.
Childhood thyroid insufficiency can cause a wide range of clinical symptoms, from mild growth irregularities to serious neurocognitive impairment. The prognosis of impacted children has been greatly improved by developments in neonatal screening, better diagnosis methods, and efficient treatment therapies.
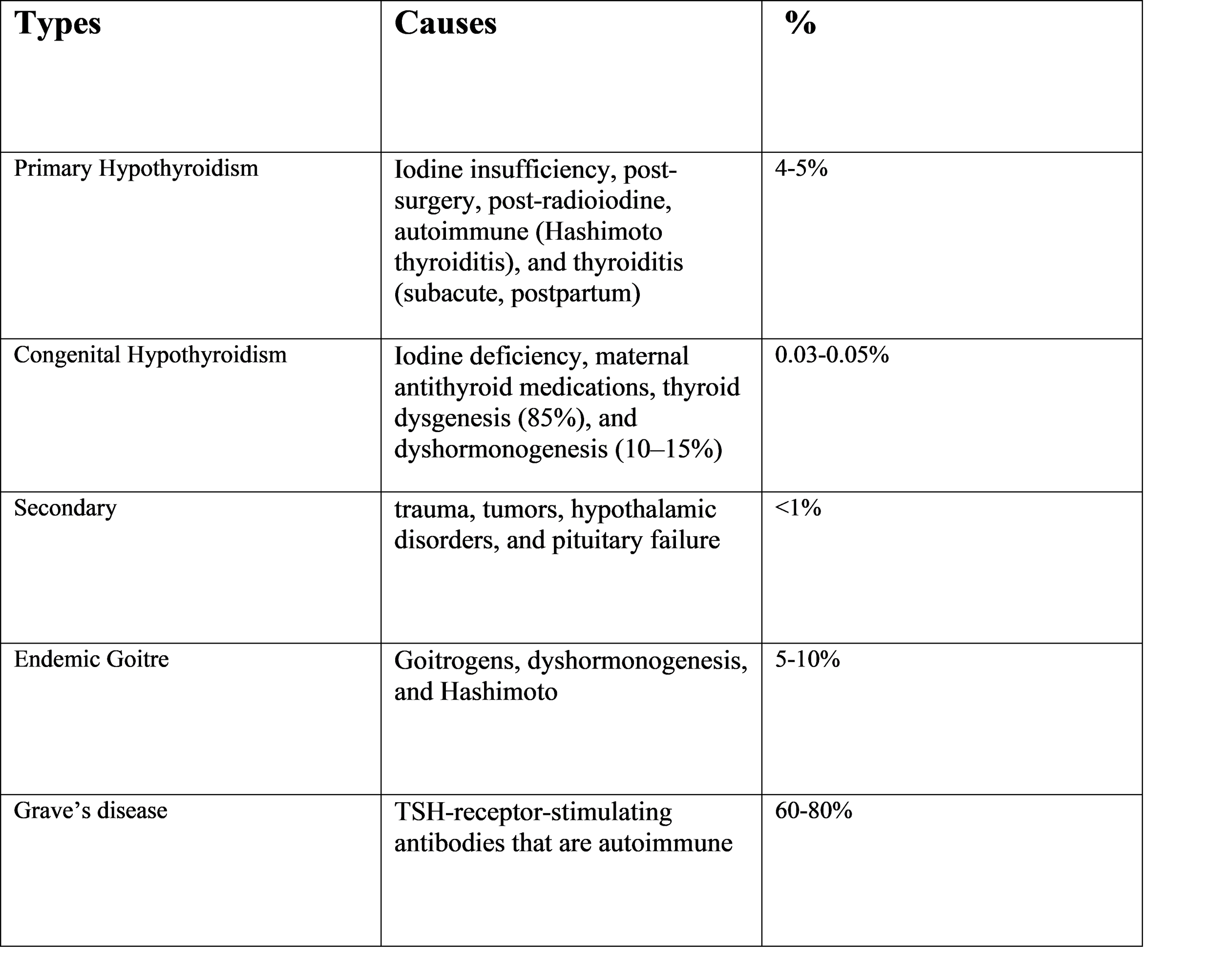
Types of thyroid gland diseases:
Endemic goiter: The swelling of the thyroid gland that occurs in communities with extensive iodine shortage is known as endemic goiter. It is still a major public health issue in many poor countries and is closely linked to environmental variables that restrict iodine availability in soil and water, goitrogen exposure, and insufficient dietary iodine consumption. Iodine deficit causes compensatory thyroid enlargement and hyperplasia because it is necessary for the production of thyroid hormones. Because it can hinder growth, cognitive development, and academic achievement, endemic goiter is particularly significant in children and adolescents. Endemic goiter still poses nutritional and developmental problems in iodine-deficient cultures, despite advancements in iodine supplementation worldwide.
Congenital Hypothyroidism: One of the most prevalent avoidable causes of intellectual impairment globally is congenital hypothyroidism, a thyroid hormone shortage that exists from birth. Since thyroid hormones are crucial for early growth, neuromaturation, and brain development, prompt identification and therapy are vital. Thyroid dysgenesis, hormone synthesis flaws, or maternal factors interfering with embryonic thyroid function can all cause the disorder. Newborn screening programs are the main means of early detection because clinical symptoms at delivery are frequently mild or nonexistent. For afflicted newborns to have typical neurodevelopmental outcomes, early diagnosis and timely commencement of levothyroxine medication are essential.
Hyperparathyroidism: Excess thyroid hormone production is the hallmark of hyperthyroidism in children, a relatively rare but clinically severe endocrine condition. Graves' disease, an autoimmune disorder caused by antibodies that activate the thyroid gland, is the most frequent cause in children. Increased sympathetic activity, accelerated development, and altered behavior are signs of excess thyroid hormone, which also affects almost every organ system and speeds up metabolic activity. In order to avoid problems including heart dysfunction, development issues, and scholastic challenges, early detection and effective care are crucial. Despite the effectiveness of treatment choices, relapse risk and treatment-related side effects necessitate rigorous long-term monitoring.
Symptoms:
1.Endemic goiter - Iodine-deficient communities are susceptible to endemic goiter.
Principal Symptoms
• Thyroid gland enlargement that is palpable or visible; typically, diffuse, smooth, and non-tender.
• Swelling in the neck that could be more apparent when swallowing
• Symptoms of compression in big goiters:
• Dysphagia, or difficulty swallowing
• Breathing difficulties (dyspnea)
• Hoarseness (caused by repeated compression of the laryngeal nerve)
• If there is a significant iodine deficit, hypothyroidism symptoms include: Weight increase, fatigue, cold sensitivity, and dry skin.
2. Congenital Hypothyroidism-
Arises from factors relating to the mother or iodine, thyroid dysgenesis, or dyshormonogenesis. Early signs (typically mild) Long-term jaundice, poor eating, lethargy or excessive drowsiness, constipation, hypothermia, big posterior fontanelle, macroglossia (large tongue), hoarse cry.
Late Symptoms (in the event of a delayed diagnosis) Growth retardation, intellectual deficiency or developmental delay, coarse facial characteristics, umbilical hernia, chilly, dry skin and bradycardia
3.Hyperthyroidism:
General Symptoms:
• Heat intolerance; • Increased sweating; • Tremor (fine); • Palpitations/tachycardia; • Weight loss despite increased hunger
Behavioral and Neuromuscular Symptoms Irritability; hyperactivity; lack of focus or deterioration in academic performance; weakening in the muscles, particularly the proximal muscles; and disturbed sleep
Skin and Eyes Proptosis, or exophthalmos; retraction or staring of the lids; and warm, wet skin.
RESEARCH METHODOLOGY
1. Study Design: Understanding the genetic, clinical, and therapeutic aspects of hemophilia—a hereditary bleeding condition brought on by clotting factor deficiencies—requires a well-structured research process. In individuals with hemophilia A, B, and c, a suitable methodological framework aids in determining the prevalence, molecular basis, clinical symptoms, and results of different treatment modalities.
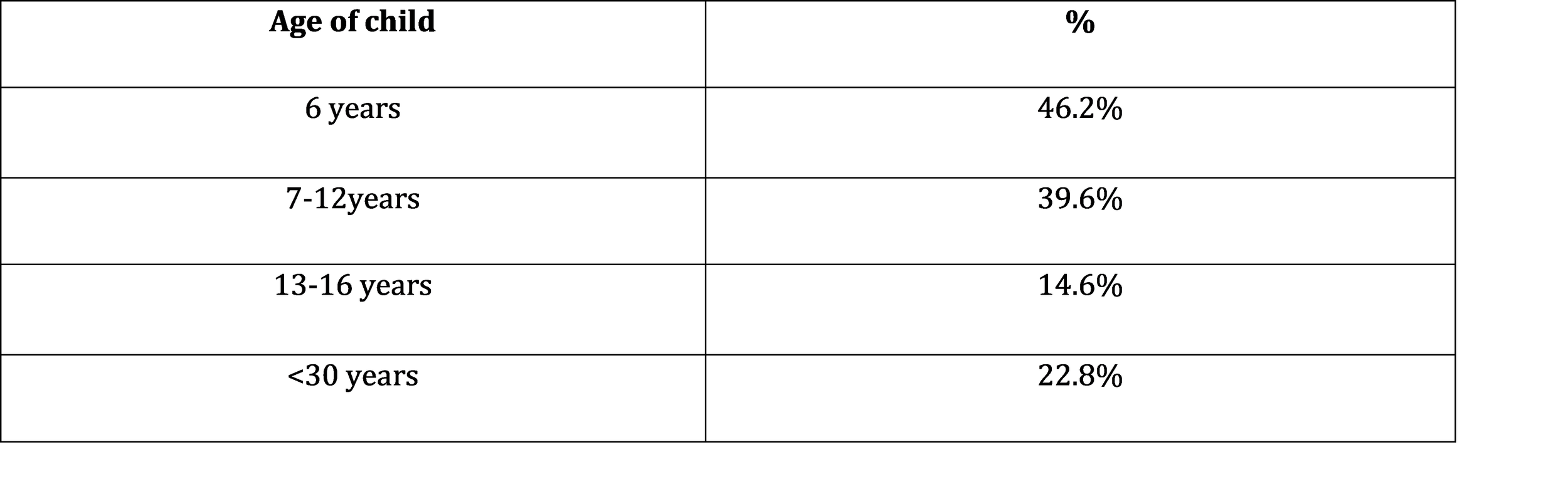
2. Study Population: Children with suspected thyroid illness between the ages of 0 and 18, regardless of gender, are eligible for inclusion. • Parents' or guardians' consent; • Exclusion criteria: • Children with systemic conditions that impact thyroid function, such as long-term liver or kidney problems • Children using drugs that change thyroid hormones, such as steroids or amiodarone
3. Sample size: The sample size was determined using normal statistical formulae based on the area incidence of thyroid problems (e.g., endemic goiter prevalence in school-aged children). • For several age groups (neonates, babies, school-age children, teenagers), stratified sampling may be employed.
4. Techniques for Gathering Data:
A. Clinical Evaluation • A thorough physical examination and history; • Screening symptoms: • Congenital hypothyroidism: persistent jaundice, hypotonia, poor eating, and macroglossia • Endemic goiter: thyroid enlargement, dysphagia, dyspnea, and exhaustion • Hyperthyroidism: palpitations, tremor, weight loss, heat intolerance, and exophthalmos
B. Research in the Lab • Thyroid function tests (TFTs): free T4, free T3, and TSH • Thyroid antibodies: TRAb (for autoimmune hyper/hypothyroidism), anti-TPO, and anti-Tg • Iodine levels in the urine (for endemic goiter) • Heel-prick TSH and T4 (for congenital hypothyroidism) test for newborns
C. Imaging Research • Radionuclide thyroid scan: optional in cases of congenital hypothyroidism or hyperthyroidism • Thyroid ultrasound: gland size, echotexture, and nodularity
5. Analysis of Data Descriptive statistics: frequency, percentage, mean ± SD for age, gender, and goiter size; chi-square or t-test comparison of prevalence across age groups and gender; correlation between biochemical results and clinical characteristics.
6. Moral Aspects Obtaining clearance from the institutional ethics committee; obtaining informed consent from parents or guardians; and ensuring patient data confidentiality
7. Measures of Outcomes The prevalence of various thyroid problems in children; the frequency of symptoms and clinical patterns; the relationship between thyroid function, laboratory results, and physical findings; and the early identification rate through screening program.
RESULT AND DISCUSSION
A 2021 global research estimated that 2.0 million people had thyroid cancer worldwide. The age-standardized prevalence rate was around 23.1 per 100,000 people worldwide (95% UI: 20.7–25.6). • Thyroid cancer was expected to have killed around 44,800 individuals worldwide in 2021 (95% UI: 39,900–48,500), with an age-standardized mortality rate of about 0.5 per 100,000. • Although mortality and DALY (disability-adjusted life years) rates have slightly decreased over the years, prevalence (i.e., number of existing cases) has increased. • New-case incidence is still significant; for example, one study estimated that there were approximately 821,214 new cases of thyroid cancer worldwide in 2022, along with 47,507 cancer-related deaths. • Women's incidence rates are much greater than men.
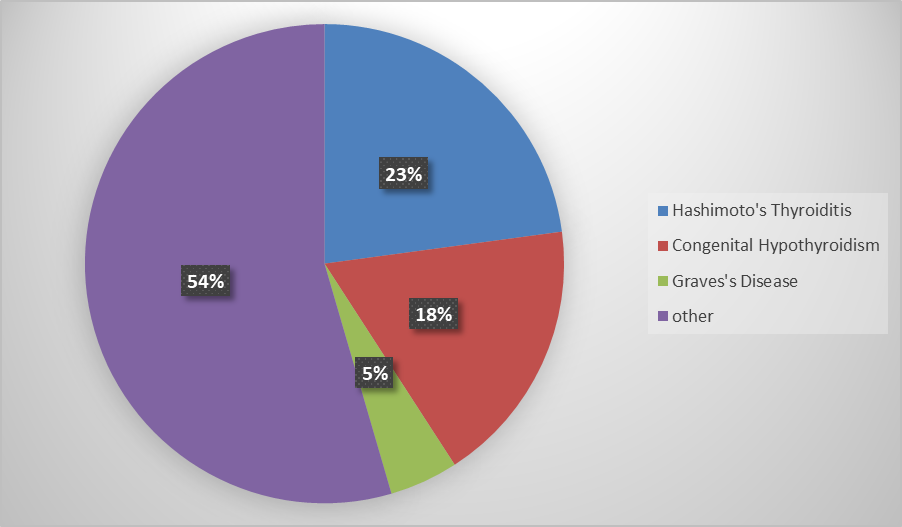
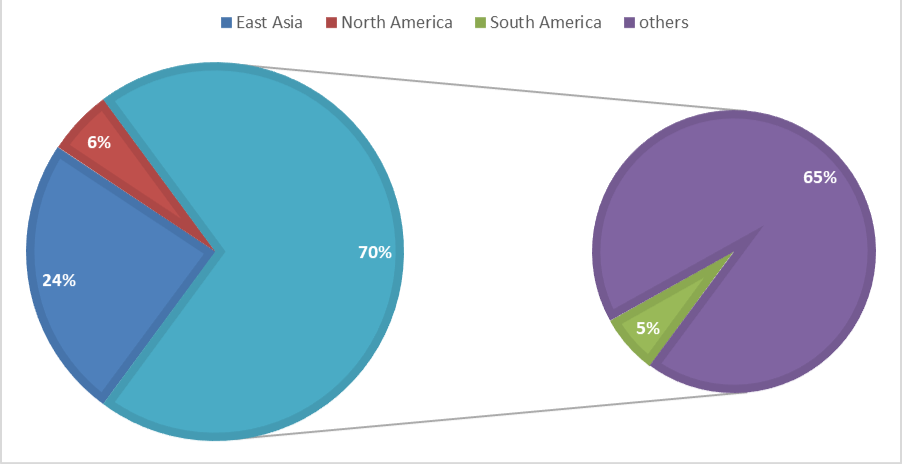
Thyroid autoimmune diseases, such as Hashimoto's thyroiditis, which frequently results in hypothyroidism • The prevalence of Hashimoto's thyroiditis (HT) was estimated to be around 7.5% worldwide by a major meta-analysis that included 48 studies and over 20 million persons. The prevalence was much greater in women (~17.5%) than in men (~6.0%). The risk for adult women is almost four times that of males. • Interestingly, the same analysis revealed that HT prevalence in adults declined over time (in the decades reviewed); however, prevalence varied widely by region: in some African populations, HT prevalence was reported to be much higher than in Asia; overall, there was high heterogeneity among studies.
By WHO, we found that, East Asia has more patient compare to others.
And in Kyrgyzstan, we found that about 72,000 neonates nationwide were screened for congenital hypothyroidism (CH) in 2023; 370 of them were determined to be afflicted. • 18 children were diagnosed with CH in pilot-screening data (from previous years) with 56,295 infants screened. This translates to approximately 1 in 3,125 births. • Based on the 1:3,125 rate from pilot data, the estimated prevalence among newborns was about 32 per 100,000 children aged 0–3 years. • For children in somewhat older age groups (school-age), a study from a region in Kyrgyzstan found that goiter (enlarged thyroid) was common among children, especially in children aged ~ 10–12 years. • In that age group, the prevalence was reported to be around 20.1%.
Currently, newborn screening is the primary source of data from Kyrgyzstan (to detect congenital hypothyroidism). Only the early stages of life are covered by it. Many additional thyroid conditions are not routinely checked for or reported for the entire kid population, such as acquired hypothyroidism, hyperthyroidism, thyroid nodules, autoimmune thyroiditis, and goiter brought on by environmental or dietary causes. There isn't a thorough national thyroid illness registry or screening program for older kids. Only specific geographical or scientific studies (e.g., on goiter prevalence) provide the published statistics. "Thyroid disease" refers to a wide range of disorders, varying greatly in incidence, age of occurrence, and severity. It would be deceptive to combine them into a single figure without complete data.
And in India, the prevalence of CH in non-endemic areas was estimated by a recent meta-analysis of numerous Indian studies to be approximately 0.97 per 1,000 live births, or roughly 1 in 1,031 neonates. In previous individual studies, some reported an incidence of 1 in 2,640 live births. In another study (in a specific region), the incidence was approximately 1.37 per 1,000 live births using cord-blood screening.
In several regions of India, these rates appear to be greater than the worldwide statistics, which frequently mention ~1 in 3,000–4,000.
Childhood and teenage thyroid conditions (goiter, hypothyroidism, hyperthyroidism, autoimmune, etc.). Of the approximately 800 children with thyroid issues in a pediatric/adolescent clinic series, approximately 79% had hypothyroidism (goitrous or non-goitrous), approximately 19% had euthyroid goiters, and approximately 2% had hyperthyroidism.
Management of Diseases of Thyroid Gland:
1.Non-drug management OF Hypothyroidism
Levothyroxine = medications (yet you requested "without drugs").
Non-pharmacological preventative and supporting strategies are included here.
A. Nutrition and Diet • Sufficient consumption of iodine (150 μg daily for adults; 250 μg daily during pregnant).
Make use of iodized salt. • Sufficient consumption of selenium (fish, eggs, and Brazil nuts).
→ Thyroid hormone conversion (T4 → T3) is supported by selenium. • Steer clear of extra goitrogens in iodine-deficient areas, such as raw cabbage, cauliflower, and cassava.
- Most goitrogens are destroyed by cooking. • Make sure you have adequate iron and zinc (deficiency exacerbates hypothyroid symptoms).
B. Way of Life • Frequent exercise enhances mood, weight control, and metabolism. • Sleep hygiene: inadequate sleep exacerbates thyroid illness.
C. Non-drug monitoring • Frequent TSH and T4 testing to track development. • Growth tracking in kids with hypothyroidism from birth.
D. Avoidance • Salt is iodized universally. • Early detection of CH through newborn screening (preventing neurodevelopmental delay).
2. Non-drug management OF Hyperthyroidism
A. Way of Life & Assistance
• If you have Graves’ disease, stay away from foods high in iodine, such as seaweed and iodinated supplements. Strict abstinence from smoking, which raises the risk of Graves orbitopathy. Stay hydrated, stay in a cool atmosphere, and avoid physically demanding activities that might cause arrhythmias.
B. Reducing stress: yoga, meditation, and relaxation techniques Graves’ disease is exacerbated by stress.
C. Modifications to nutrition • Consuming enough calories (people with hyperthyroidism lose weight). • Enough calcium and vitamin D to prevent bone loss. • Steer clear of stimulants like energy drinks and coffee.
3. Non-drug management of goiter (enlarged thyroid)
A. Nutritional/Endemic Goiter Supplementing with iodized salt. • Boost iodine levels in meals (dairy, eggs, and shellfish). • Address contaminated water since thiocyanates prevent iodine from being absorbed. • Steer clear of too many goitrogenic foods.
B. Not endemic Goiter • The use of ultrasound. • Steer clear of needless iodine supplements. • Keep an eye out for growth and steer clear of neck pressure (tight clothing).
C. Non-pharmacological Surgical Treatment
Indications include: • compression from a large goiter; • rapid growth; • cosmetic grounds; and • suspicion of cancer.
4. Non-Drug Treatment of Thyroid Nodules
A. Observation • For benign nodules, many patients just need: • TSH monitoring → Annual ultrasound • Steer clear of needless iodine supplements
B. Lifestyle • Prevent neck radiation exposure • Consume enough iodine
C. Non-pharmacological, minimally invasive techniques: radiofrequency ablation (RFA); ethanol ablation (percutaneous ethanol injection); laser ablation used to treat solid or benign cystic nodules.
COMPLICATIONS
1. Hypothyroidism, either acquired or congenital
A. Congenital hypothyroidism; growth retardation or dwarfism; delayed bone age or skeletal maturation; hearing impairment; coarse facial characteristics if severe; neurodevelopmental delay → mental retardation if untreated
B. Acquired hypothyroidism; • Myxedema, which causes extreme skin and tissue swelling; • Myxedema coma, which can be fatal and is brought on by an illness, cold, or shock; • Cardiovascular problems; • Bradycardia; • Pericardial effusion; • Heart failure Infertility and irregular menstruation; peripheral neuropathy and carpal tunnel syndrome; hyperlipidemia and an elevated risk of atherosclerosis; goiter enlargement and airway blockage
2. Hyperthyroidism:
A. Graves' illness Thyroid storm: an abrupt hypermetabolic condition that can be fatal; cardiovascular issues • Heart failure; tachyarrhythmias (AFib in adults) • Osteoporosis leads to a higher risk of fracture; • Exophthalmos or ophthalmopathy leads to visual issues; • Pretibial myxedema; • Muscle weakness or wasting; • Malnutrition, weight loss
B. Toxic Nodular Goiter/Toxic Adenoma • Graves-like consequences, with the exception of ophthalmopathy
3. Goiter, dysphagia (difficulty swallowing), dyspnea (difficulty breathing), hoarseness (recurrent compression of the laryngeal nerve), and superior vena cava syndrome (rare, extremely big goiter) • Malignant transformation (rare in multinodular goiter); • Cosmetic deformity and social stigma
4. Thyroid Nodules • Cancer → About 5–15% of nodules may be malignant; compression symptoms (big nodules); dysphagia, dyspnea, and hoarseness; and cosmetic issues
5. Thyroid cancer with local invasion of the trachea, esophagus, and recurrent larynx Metastasis; regional lymph nodes; papillary and follicular lungs; medullary and follicular bones; hypoparathyroidism following surgery (low calcium, tetany); and recurrent laryngeal nerve damage leading to hoarseness or vocal cord paralysis
CONCLUSION
Thyroid gland diseases include a broad range of conditions that can impact people of all ages, from young children to the elderly. Through the production of the hormones T3 and T4, the thyroid gland is essential for controlling growth, development, and metabolism. Growth retardation, neurodevelopmental delay, weariness, weight gain, and, in extreme situations, myxedema or myxedema coma can result from hypothyroidism, whether it is congenital owing to thyroid dysgenesis or dyshormonogenesis or acquired via autoimmune illness, iodine shortage, or surgical procedures. Weight loss, heat intolerance, tremors, palpitations, osteoporosis, and in Graves' disease, ophthalmopathy are symptoms of hyperthyroidism, which is most frequently brought on by toxic nodular goiter, thyroiditis, or Graves' disease. Thyroid storm and arrhythmias are possible side effects.
While thyroid nodules carry a risk of malignancy and thyroid cancers, though relatively uncommon, can invade locally or metastasize, necessitating surgical and occasionally radioactive iodine interventions, goiter, which frequently results from iodine deficiency, can cause airway or esophageal compression and cosmetic concerns. Subacute, postpartum, and autoimmune forms of thyroiditis can cause temporary thyrotoxicosis, hypothyroidism, and in rare cases, thyroid cancer. Thyroid disorders are major public health issues worldwide; hypothyroidism affects around 4–5% of the population, hyperthyroidism 1-2%, and goiter up to 15%, with greater incidence in iodine-deficient areas; congenital hypothyroidism affects about 1 in 2,000–3,000 births.
Neonatal screening has identified a significant number of afflicted children in nations like Kyrgyzstan and India, highlighting the significance of early identification and preventative measures like iodized salt supplementation. Untreated thyroid diseases can lead to serious consequences, such as poor quality of life, development, puberty, and reproductive outcomes; neurocognitive impairment in children; cardiovascular disease; metabolic disorders; and life-threatening situations such myxedema coma and thyroid storm. Preventive measures, dietary and lifestyle changes, pharmacologic therapy when needed, and surgical procedures for compressive or malignant disease are all part of management, which emphasizes the importance of prompt diagnosis and all-encompassing care to lower morbidity and long-term complications.
REFERENCE
1. The Thyroid and its Diseases: A Comprehensive Guide for the clinician (2019, Springer)
2. Thyroid Disease: Pathogenesis, Diagnosis and Treatment (2018, springer)
3. Thyroid Disease: A Case-Based and Practical Guide for Primary care by Emanuel O. Brams (2005)
4. Diseases of the Thyroid (contemporary Endocrinology series, ed. Braverman, 1990s)
5. Thyroid and Parathyroid Disorder in children: A Practical Handbook (2021)
6. Nuclear Medicine in Endocrine disorders: Diagnosis and Therapy (2022)
7. Hand and Neck Endocrine Surgery: A Comprehensive Textbook, Surgical and Video Atlas (2021)
8. Pediatric Thyroidology (2014)