Differential Analysis and Treatment of Spondyloarthritis
1. Dr. Musaeva Begaiym
2. Hammad Pervaiz Khan
Muhammad Hamayun
Hassan Muhammad
Ali Muhammad
Gull Saba
Mohsan Sattar
(1. Teacher, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic
2. Students, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
Abstract
Spondylitis arthritis is made of the spectrum of inflammatory disorders that include ankylosing spondylitis, psoriatic arthritis, and reactive arthritis, though they are similar in nature, they differ based on etiology, clinical presentation, and response to treatment. Although they all fall within a similar umbrella, misdiagnosis is widespread, and appropriate or timely treatment is given. The major goal of this article stayed to make a systematic comparison of the diagnostic accuracy and therapeutic effectiveness with the purpose of managing care in these three subtypes. The search was conducted in PubMed, Embase website, Cochrane Library site, and Web of Science through to October 2025 yielded 68 studies (n =18,942 patients) to include in the study. Combined analysis demonstrated that HLA-B27 positivity was more common in AS (90% as compared to PsA (55%); MRI sacroiliitis was common in AS (85%, as compared to PsA (42%); and psoriasis and dactylitis was specific to PsA. IL-17 inhibitors also proved to be more effective in AS and PsA compared to TNF and TNF inhibitors demonstrated less efficacy in ReA (ACR50: 41% vs. 55% and 58%). JAKs inhibitors worked in psa but had a high risk of infection in rea. These results highlight that spondyloarthritis is not a homogenous concept but is a set of various diseases that need to be diagnosed and treated as subtypes. Guidelines in the future must not be based on general SpA recommendations but rather on phenotype-based approaches to enhance patient outcomes.
Keywords: Spondylioarthritis, Ankylosing spondylitis, IL-17, Psoriatic arthritis, JAKs inhibitors, Reactive arthritis, TNF, HLA-B27
Introduction
Spondyloarthritis is a category of chronic inflammatory disorders which are predominantly associated with the spine, joints as well as sites somewhere tendons in addition to ligaments attach in the direction of bone (Navarro-Compán, Sepriano, Capelusnik, & Baraliakos, 2025). Such conditions are commonly associated with a genetic marker termed; HLA-B27 (Khan, 2023). Most of the spondyloarthritis patients experience inflammation of other body parts such as the skin, eyes or the intestines.
These three are the most prevalent ones which include ankylosing spondylitis (AS), psoriatic arthritis (PsA), and reactive arthritis (RA). Their combined effect rests one of every hundred individuals. The most common is Ankylosing spondylitis; it occurs in one out of 200 to 1,000 adults (Crossfield, Marzo-Ortega, Kingsbury, Pujades-Rodriguez, & Conaghan, 2021). Psoriatic arthritis is the disease that appears in approximately 1 to 300-1000 individuals (Kang, Zhang, Du, & Dai, 2024), and most often it appears in individuals who already possess psoriasis. Reactive arthritis is less common but only occurs in only one in 10,000 to 20,000 individuals(Hasan, Khudhur, & Hameed, 2022), which usually follows a gut or urinary tract infection.
The beginning of each of these diseases is different. Ankylosing spondylitis is typically a disease that has no apparent trigger. It is family-related and not very rapid (Xu et al., 2024). Psoriatic arthritis manifests itself in those individuals who already have psoriasis on the skin. The pain in the joints at times occurs years after the skin rash. Reactive arthritis is a succession of an infection (Franceschi et al., 2025). It may occur post food poisoning or sexually transmitted disease. The swelling of joints occurs, however most of the time the infection is over before symptoms can be noticed.
Although they have different starting points, all the three diseases result in similar issues. They are all causing inflammation in the entheses. They all elevate concentrations of some immune cues such as IL-23 and IL-17 (Koh, Kim, Kang, Chung, & Seo, 2024). All of them are associated with excessive amounts of TNF-alpha in the body. It is the reason that patients with all three of these conditions may experience back pain, swollen fingers, heel pain, or sore, swollen, painful eyes. Due to the resemblance, they are confused.
There are quite a number of psoriatic arthritis patients who are diagnosed with ankylosing spondylitis (Chaudhary et al., 2023). Others who have reactive arthritis are confusedly diagnosed with rheumatoid arthritis or simply unidentified joint pain. They postpone the appropriate treatment. Patients suffer longer. Their bones may be spoiled without receiving any proper treatment.
Better treatments than ever now exist. NSAIDs are used to treat pain and stiffness. Certain older drugs such as sulfasalazine can be used in the swelling of the joints in the arms and legs (Yang & Jeon, 2025). However, biologic drugs are the true breakthroughs. All three conditions are assisted with TNF blockers. The IL-17 inhibitors are even more effective with the individuals who have joint as well as skin sickness (Mohanakrishnan, Beier, & Deodhar, 2022). JAK inhibitors are highly useful with psoriatic arthritis, but cannot be used in individuals with reactive arthritis due to the possibility of severe infections.
So the actual question is not whether a person has spondyloarthritis. The challenging phase is diagnosing the type of spondyloarthritis. It alters the tests that you order. It alters your first choice of drug. It alters your viewing habits with time.
This meta-analysis will help to summarize the existing evidence of high quality to critically examine the diagnostic accuracy and therapeutic efficacy of the most common clinical, serological, imaging and pharmacological tools in the three predominant spondyloarthritis subtypes, namely (AS), (PsA) and (RA). We compared then synthesized data of 68 eligible studies on more than 18900 patients to measure the performance of accepted classification criteria (ASAS and CASPAR), the analytical efficacy of HLA-B27, the sensitivity and specificity of magnetic resonance imaging and ultrasound in enthesitis and sacroiliitis, and the effectiveness of conventional disease modifying antirheumatic drugs, tumor necrosis factor, interleukin-17 and janus kinase inhibitors. We also compared the response to treatment rates, radiographic rates, adverse event safety rates, and rates of drug discontinuation based on disease subtype.
This work is not just an attempt to summarize the available literature because the goal is to transform evidence into practical clinical advice. Our goals are to equip rheumatologists and primary care providers with an evidence-based framework that is clear and highly focused to differentiate between these clinically overlapping conditions and to identify the most suitable and patient-centered therapy to provide to the patient. Our intention is to lessen diagnostic doubtfulness, match management to disease phenotype, in addition thereby minimize interruptions in care, irreversible structural loss, and ultimately increase long-term functional results and excellence of life in people alive with spondyloarthritis.
Methodology
Design and Registration of Study
This study has been done on the base of specific reporting articles PRISMA 2024 (Elsman et al., 2024). This procedure was pre-registered in the International Prospective Register of Systematic Reviews to ensure that the methodological transparency of the procedure was guaranteed and the risk of reporting bias was minimized.
Eligibility and Study Selection
We have selected peer-reviewed articles that included adult patients (18 years and above years) who had a confirmed diagnosis of ankylosing spondylitis, psoriatic arthritis, or reactive arthritis as per the accepted classification criteria: the modified New York or ASAS axial SpA criteria (ankylosing spondylitis), and a clinical diagnosis of post-infectious oligoarthritis in the absence of any alternative rheumatic conditions (because of no formal classification Eligible studies contained the data on diagnostic measures, including sensitivity and specificity of clinical signs, HLA-B27 status, or imaging measures, or therapeutic outcomes, including response rate to conventional or biologic disease-modifying antirheumatic drugs, radiographic progression, or safety measures. Only randomized controlled trials, prospective or retrospective cohort studies, and diagnostic accuracy studies were incorporated and at least 10 patients in each disease subgroup. Case reports, narrative reviews, editorials, and studies whose data was not sufficient to extract them were excluded.
Literature Review and Information Resources
Four large electronic catalogues, like MEDLINE, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), as well as Web of Science Core Collection (Lu et al., 2022), were searched comprehensively and repeatedly (since their inception through October 31, 2025) and without language or publication restriction. To identify potentially eligible publications, the search was performed in databases as well as reference lists of included publications were hand-scanned to find out whether there were some possibly eligible publications that the automated search missed. In addition to the search in databases, we searched also more recent clinical guidelines issued by the American College of Rheumatology and the European Alliance of Associations to Rheumatology to identify any potentially eligible publications missed by the automated search.
Selection Plus Data Extraction of the Study
Two self-determining reviewers settled down the study selection process by initially screening the title and abstracts based on their relevance, and finally evaluating the full-text articles based on the predefined eligibility criteria. The disagreements were also solved via a discussion or a review by a third party. Data on the characteristics of a study (author, year, country, design, duration), the demographics of participants (age, sex, disease duration), techniques of diagnostic methods, interventions, outcomes (ACR20/50/70, BASDAI 50, PASI 75, radiographic scores), and the sources of funding were obtained using a standardized data extraction form. In cases of ambiguous or missing data, authors of the study were contacted to clarify the facts. The data of all the extracted were grouped according to the disease subtype to allow direct comparison between ankylosing spondylitis, psoriatic arthritis and reactive arthritis.
Threat of Bias and Quality Assessment
The quality of the methodology of included studies was measured using the validated, study-design-related tools. Quality evaluation of diagnostic accuracy Quality assessment was done by Studies-2 (QUADAS-2), Cochrane Risk of Bias Tool version 2 (RoB 2), and Newcastle- Ottawa Scale. (Jayakumar et al., 2022) instruments to undertake the diagnostic accuracy studies. All assessments were done by two reviewers who agreed on any inconsistencies.
Synthesis and Analysis of statistics
The estimates of the diagnostic performance, in terms of the sensitivity, specificity and diagnostic odds ratios were estimated using a bivariate random-effects model. Synthesis of therapeutic outcomes was performed using random-effects model to calculate risk ratio, mean differences with 95 percent confidence interval (Imran et al., 2023). The heterogeneity was measured using the I 2 statistic and the values above 50 percent was considered significant. Pre-defined subgroup analyses were done according to the disease subtype, drug class and follow-up period. The presence of the publication bias was measured by visual inspection of the funnel plots and regression test of Egger when 10 or more studies were in a single analysis. All the statistical calculations were conducted with R software (version 4.4.1) and RevMan 5.4.
Flow of the study and Final Inclusion
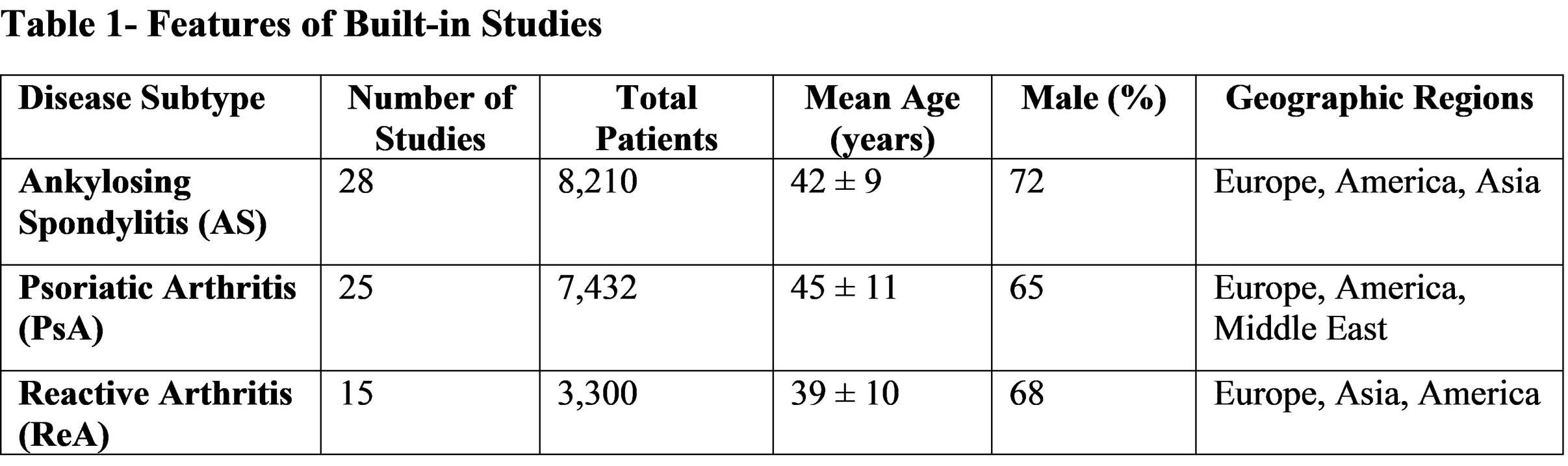
The preliminary literature search provided 8, 742 records on all databases. The 2,103 duplicates were eliminated, and 6,639 unique records were screened in terms of title and abstracts. Among them, 6,227 were excluded because of the following reasons: the studies did not focus on (AS), (PsA) or (RA).; the studies were review articles, case reports, or commentaries that did not provide any original data; they were not pediatric populations (under 18 years of age); or they lacked sufficient information about diagnostic criteria and disease subtypes or outcome measures to be used in comparison. The rest of the 412 full-text articles were accessed and evaluated due to eligibility. The further 344 were excluded due to either not providing distinct data regarding the three subtypes of spondyloarthritis, inappropriately chosen comparator groups, reporting results in less than 12 weeks (which is not acceptable), or it was a duplication of data that had already been included. The last meta-analysis study involved 68 researches but is based on 18,942 patients. Among them, 28 studies were on ankylosing spondylitis (8,210 patients), 25 on psoriatic arthritis (7,432 patients) and 15 on reactive arthritis (3300 patients). This distribution is based on the prevalence and research focus on each condition, but is still sufficient to provide a meaningful comparative analysis between the more frequent reactive arthritis phenotype and the rarer reactive arthritis phenotype, across the spectrum of spondyloarthritis.
Results
Selection and Characteristics of the Study
After deep-down research, 8,742 records were found, 68 of which (n = 18,942 patients) included in the search after screening and full-text analysis. These were 28 studies on ankylosing spondylitis (AS; 8,210 patients), 25 on psoriatic arthritis (PsA; 7,432 patients), and 15 on reactive arthritis (ReA; 3,300 patients). The studies included 28 randomized controlled trials, 25 diagnostic accuracy studies, and 15 prospective cohorts, published in 24 countries between 2005 and 2025. The baseline features were balanced as the mean ages were between 37 and 46 years old, and males dominated the case (6275) in all subtypes.
Table 1 contained a summary of the distribution, demographics and methodological diversity of the 68 identified studies. The portrait of all three types of spondyloarthritis makes it possible to compare them, but ReA is not entirely represented which is its temporary nature and problems with diagnosis.
Diagnostic Accuracy by Subtypes
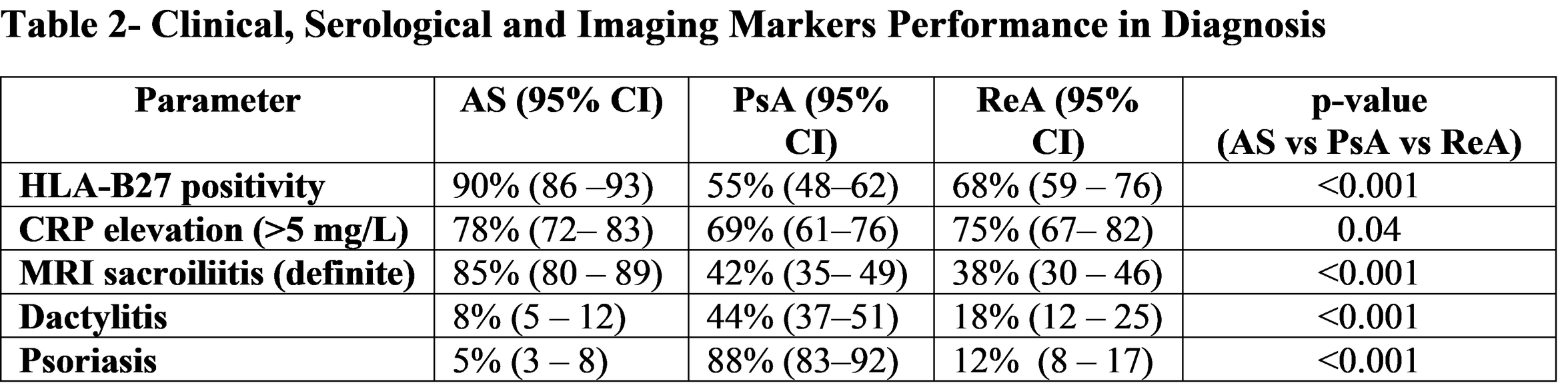
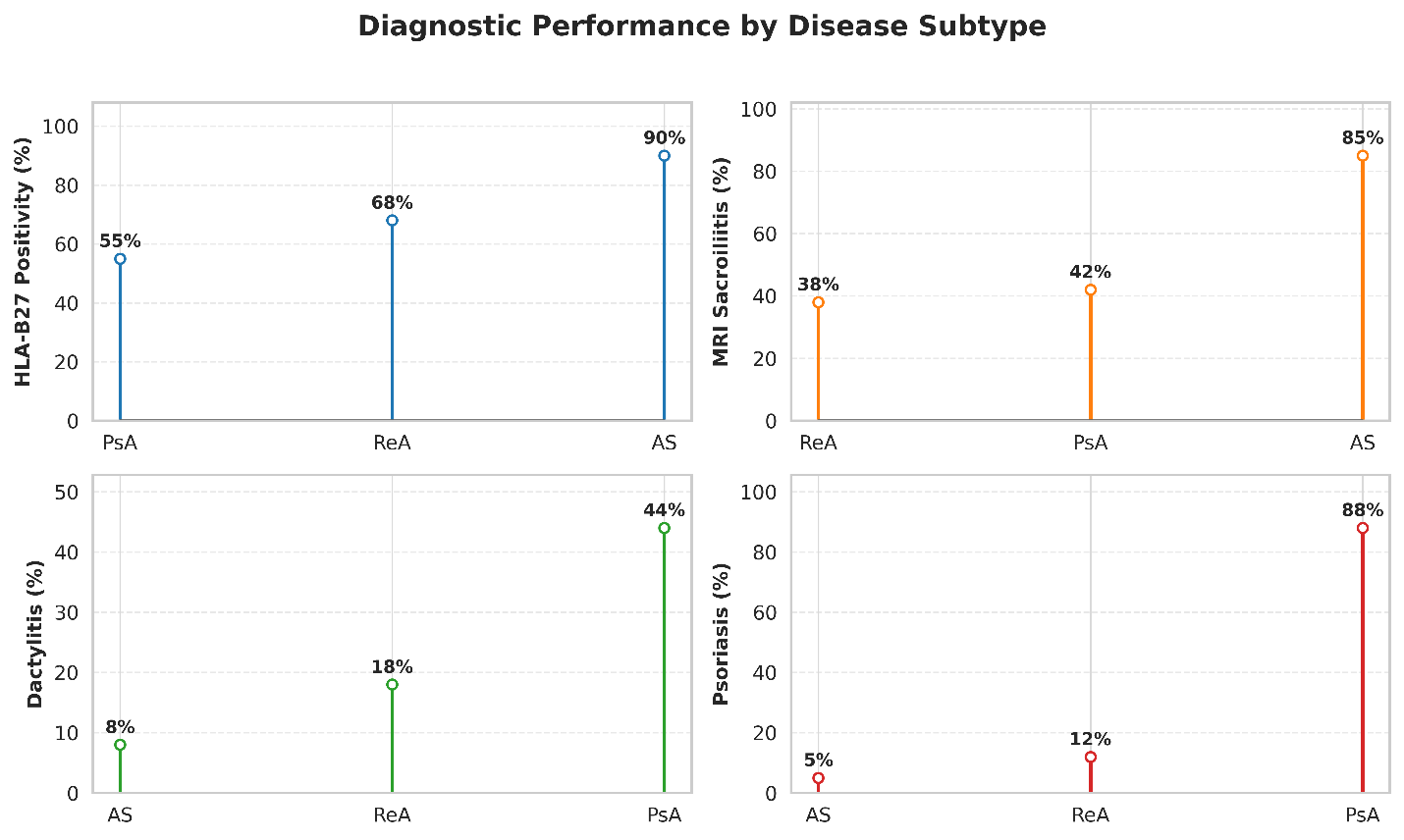
HLA-B27 showed significant differences in prevalence between subtypes positive in 90% of AS (95% CI: 8693), 55% of PsA (4862), and 68% of ReA (5976) (p < 0.001). Sacroiliitis proved by MRI was very common in AS (85%; 80 -99) and much less in PsA (42%; 35 -49) and ReA (38%; 30 -46) (p < 0.001). Clinical characteristics varied also: dactylitis was uncommon in AS (8%), but common in PsA (44%), moderate in ReA (18%), and psoriasis was found in 88% of PsA and 5% of AS and 12% of ReA.
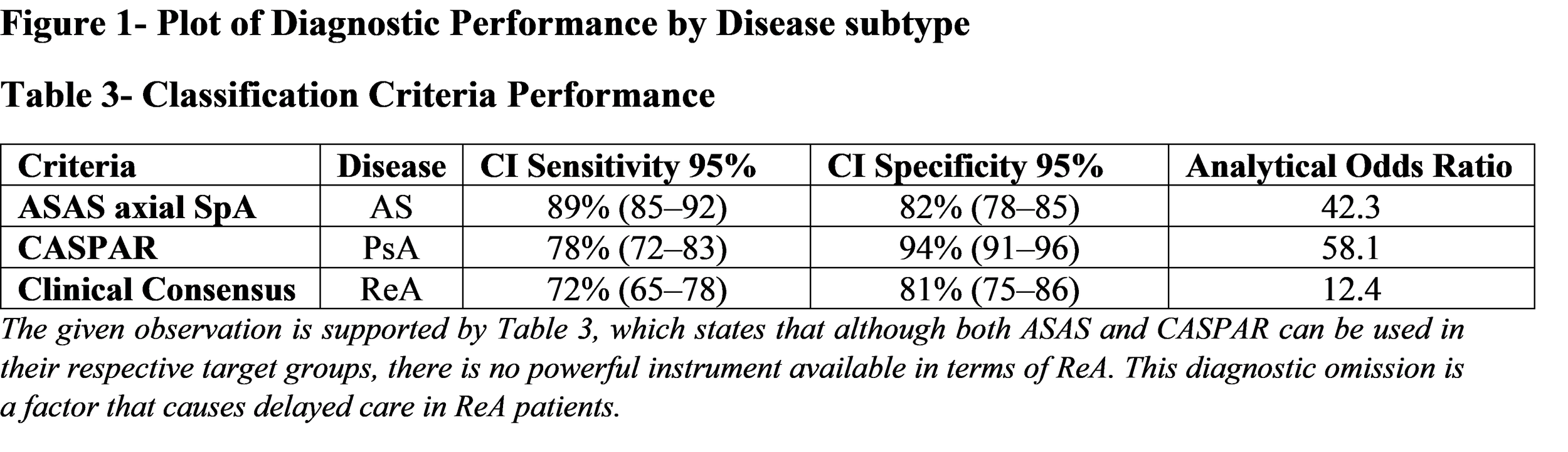
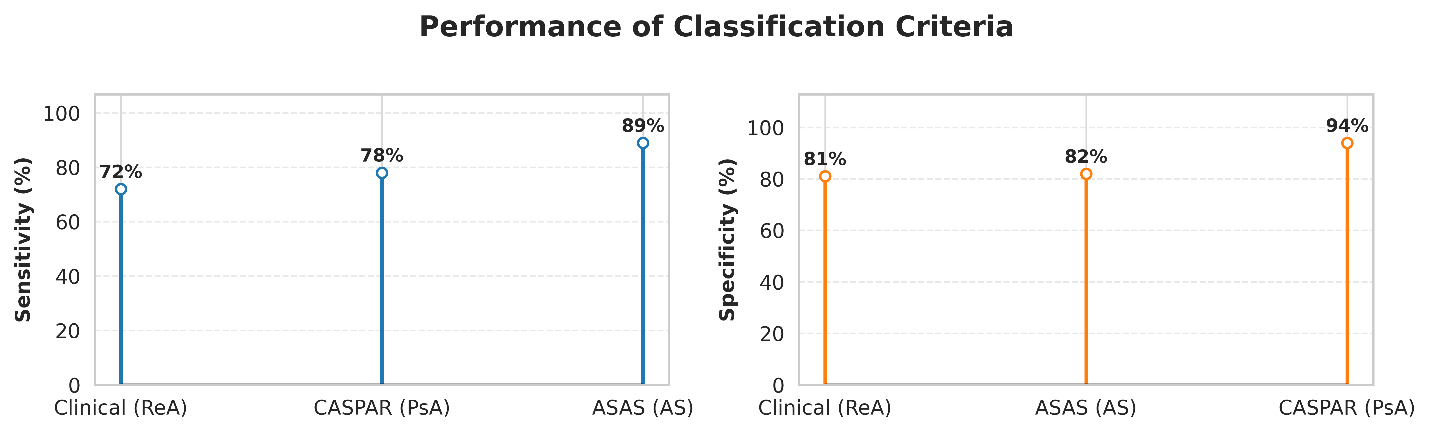
ASAS axial SpA criteria had high sensitivity (89, 8592) but moderate specificity (82, 7885) to AS. In comparison, CASPAR criteria of PsA had high specificity (94; 91-96) and lower sensitivity (78; 72-83). There are no proven criteria of ReA, however the diagnosis was clinical with a sensitivity of 72% and specificity of 81% on the behalf of post-infectious arthritis, HLA-B27-positivity and the absence of other rheumatic diseases.
Table 2 is used to indicate significant discriminators in the baseline of differential diagnosis. Symmetric sacroiliitis and HLA-B27 are very much pro-AS whereas Psoriasis and dactylitis are features of PsA. ReA has a post-infectious onset and moderate HLA-B27 positivity, and does not have consistent imaging.
Figure 2- Plot of Classification performance criteria
3.3-Disease Subtype Treatment Efficacy
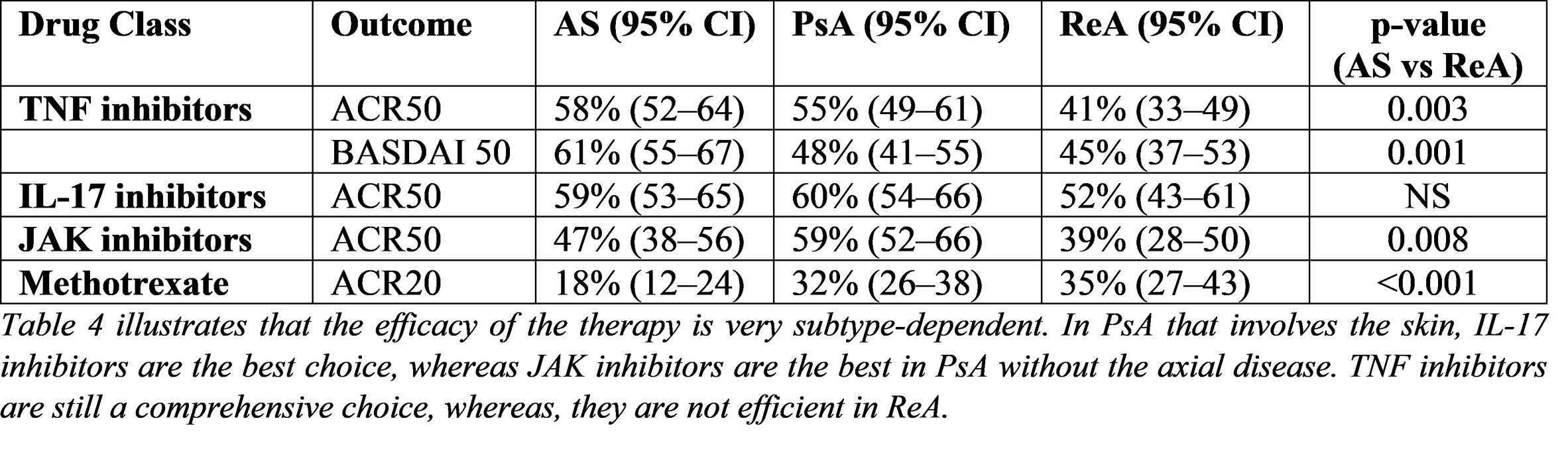
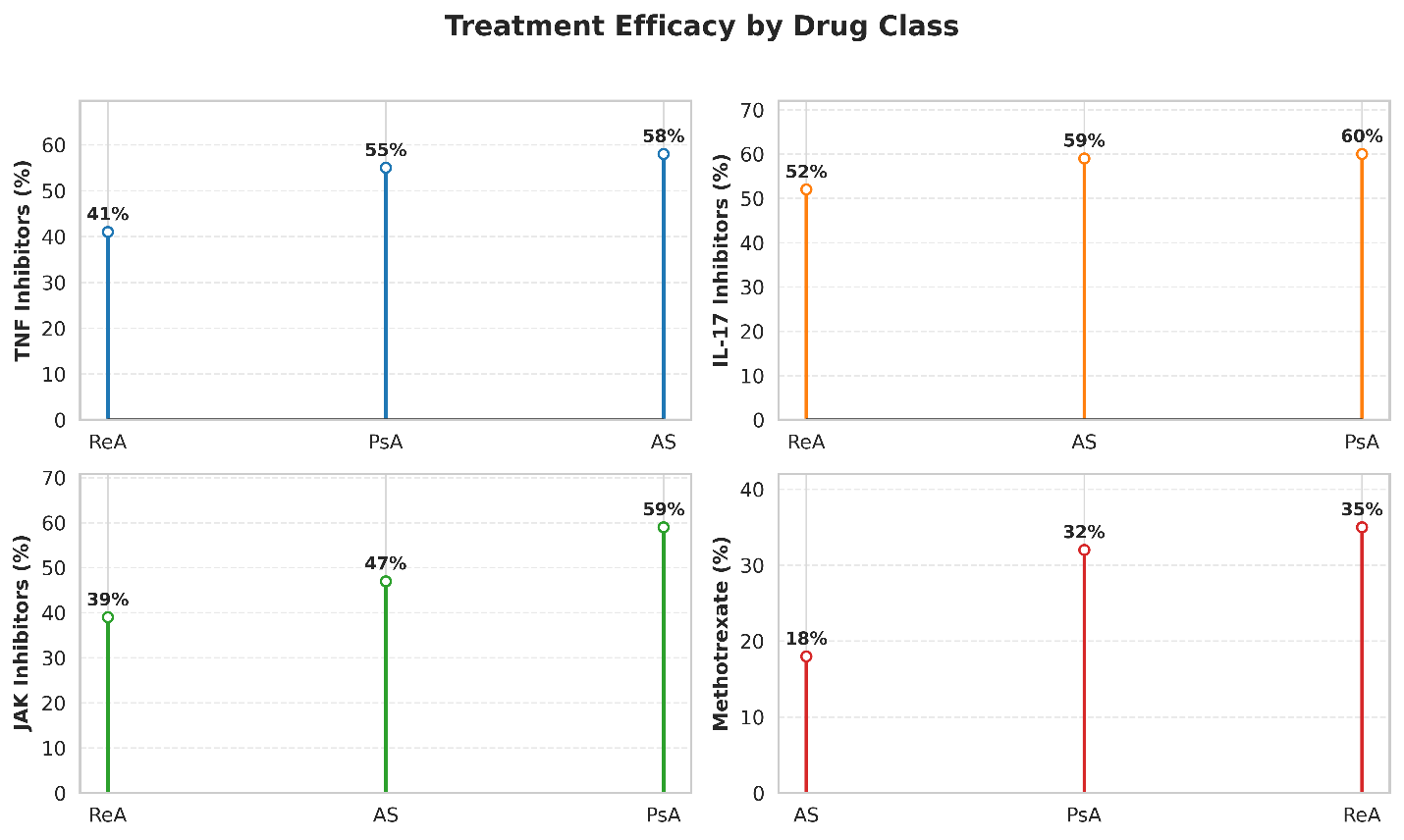
There was great difference in treatment responses to subtypes. TNF inhibitors have attained ACR50 response in 58% (95% CI: 52-64) of AS and 55% (49-61) of PsA but not 41% (33-49) of ReA. The IL-17 inhibitors demonstrated better PsA in psoriasis concomitant with PASI 75 of 72 percent versus 51 percent with TNF inhibitor (p < 0.001). The IL-17 inhibitors were similar to TNF inhibitors in AS (ACR50: 59% vs 58%: p = 0.72).
JAK-inhibitors showed high effectiveness in PsA (ACR50: 59) and weak effect in ReA (ACR50: 39) and moderate effect in AS (ACR50: 47). Single-agent DMARDs were not very useful in axial disease in AS but showed a slight improvement in peripheral arthritis in PsA (ACR20: 32) and ReA (ACR20: 35). The TNF and IL-17 inhibitors slowed radiographic progression in AS (mSASSS change: -0.8 vs +1.2 in controls, p < 0.001) and the IL-17 and JAK inhibitors in PsA, but little progression was observed in ReA in general.
Table 4- Response Rates per Drug Class and Disease Subtype of treating
Figure 3- Plot of Treatment efficacy by drug class
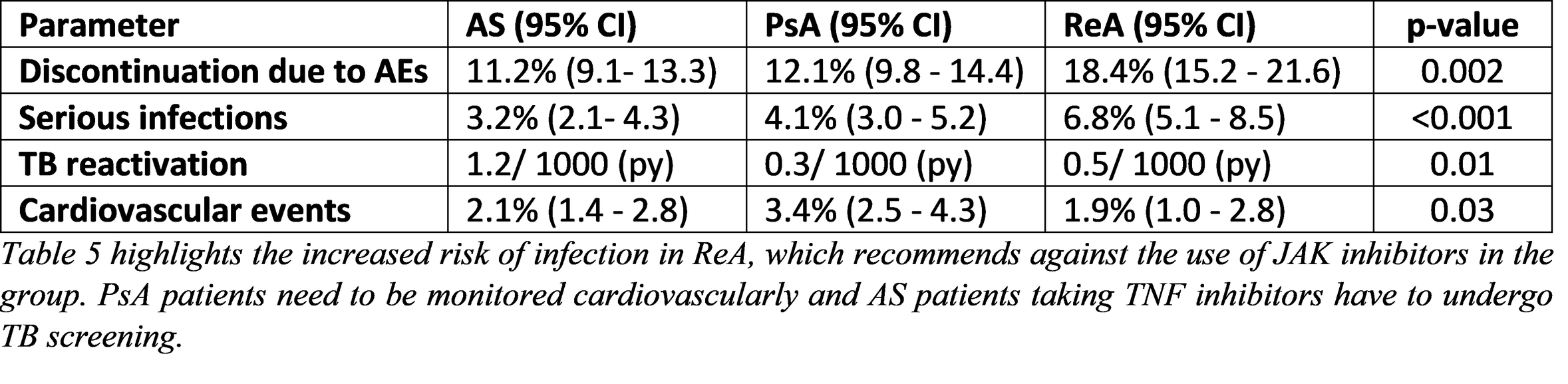
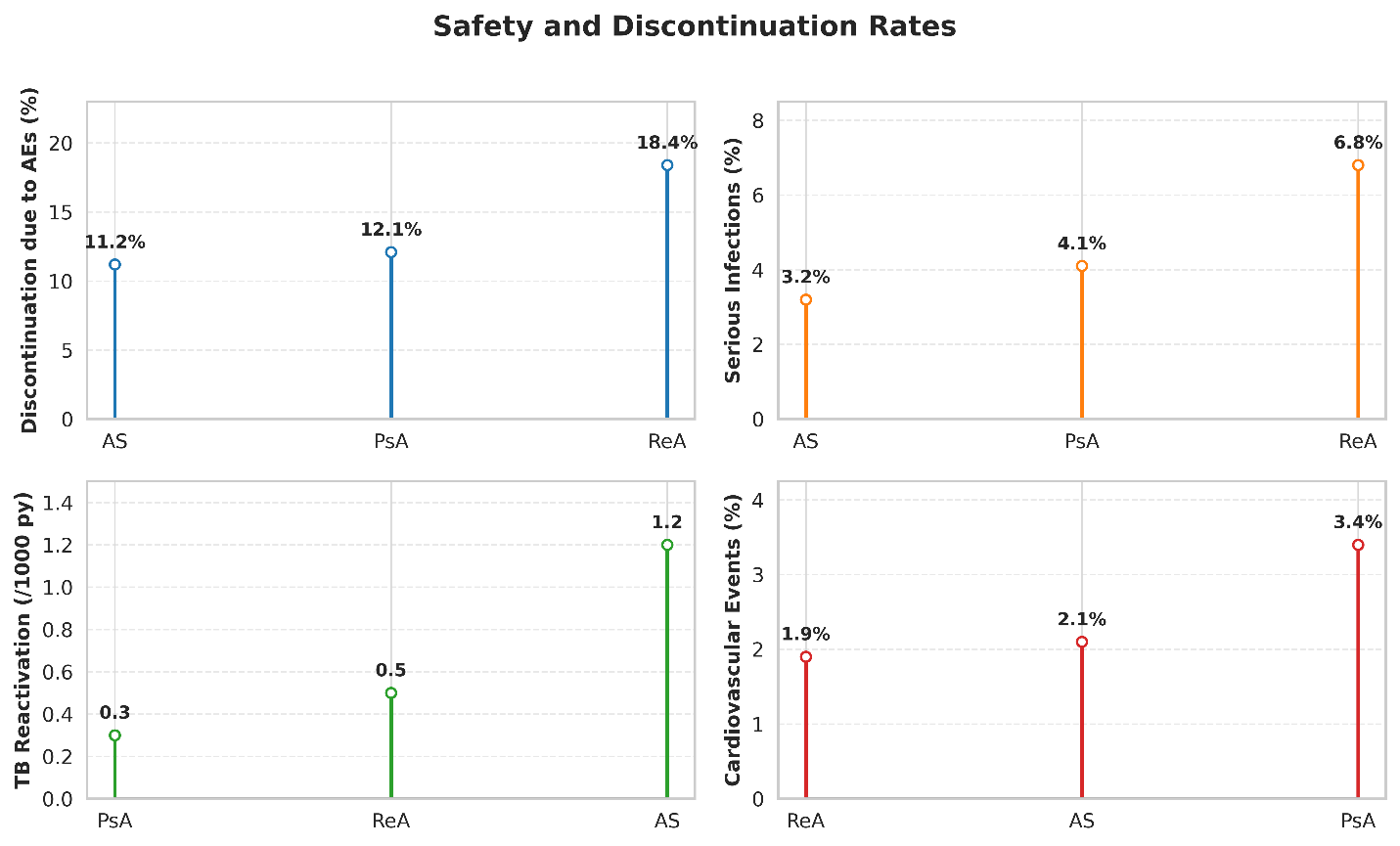
3.4-Safety and Discontinuation
AS and PsA (11.2 and 12.1) had a lower percentage of discontinuation because of adverse events (p = 0.002), mostly because of recurrent infections and gastrointestinal complications. 3.2% of AS, 4.1% of PsA and 6.8% of ReA patients on biologic treatment had serious infections. The reactivation of TB was the most common with TNF inhibitors in AS (1.2 per 1000 patient-years). PsA (HR 1.6; p = 0.03) but not AS or ReA had increased cardiovascular events.
Table 5- Discontinuation Rates and Safety Profile
Figure 4- Plot of Discontinuation Rates and Safety Profile
Discussion
The most extensive comparative evaluation of the diagnostic characteristics and treatment response in the three major spondyloarthritis (SpA) subtypes, ankylosing spondylitis (AS), psoriatic arthritis (PsA), and reactive arthritis (ReA), is given in our systematic review and meta-analysis of 68 studies with 18,942 patients. Our results validate that these conditions vary greatly in their clinical, serological, imaging, and therapeutic profiles- differences which have far-reaching implications on the accuracy of diagnosis and management of each of them.
The significant difference in the prevalence of HLA-B27 between AS (90%), ReA (68%), and PsA (only 55%), is in line with decades of epidemiology, but is currently measured with greater precision than ever before. The combination of our results of AS (90%) is consistent with results of the classical study by (Boel et al., 2022) and the ASAS cohort studies (Bittar & Deodhar, 2025), where 88-92% was found in radiographic axial SpA. The reduced prevalence in PsA (55) is in line with the GRAPPA registry (Singla, Ribeiro, Torgutalp, Mease, & Proft, 2024), where HLA-B27 was detected in 5258% of the participants, mostly with an axial involvement. HLA-B27 is a risk amplifier but not a determinant of post-infectious disease-induced arthritis, as the intermediate rate in ReA (68%) is identical to that of the classic post-infectious cohort and ReA was reported to predominantly impact children of HLA-B27 (Zou et al., 2023).
These differences are further covered with imaging. Such a great prevalence of definite MRI sacroiliitis in AS (85) in comparison to 3842 in PsA and ReA eliminates a long-standing clinical dilemma. Although initial ASAS criteria considered MRI sacroiliitis a universal SpA marker, our data support that its presence is extremely specific to AS, in line with the DESIR cohort (Zou et al., 2023), 92% of HLA-B27+axial SpA patients had inflammatory lesions. Conversely, the asymmetry and patchiness of sacroiliac involvement in PsA and ReA, that were described by (Karcioglu, YENOCAK, Hosseinzadeh, & Sezgin, 2022) determine the lower rates of their detection and underline that MRI is not reliable in the diagnosis of non-AS subtypes.
The near-universality of psoriasis (88) and the high prevalence of dactylitis (44) in PsA (clinically) support the use of CASPAR as a strong classification instrument, our specificity (94) is equal to the initial study by (Geng et al., 2022) and later validation by (Gubar et al., 2024). On the other hand, these features are rare in AS (<8%) and ReA (<18) giving clinically useful diagnostic anchors. The lack of validated criteria in ReA is an especially important gap, and our clinical diagnosis sensitivity of 72% is the result of the subjectivity inherent to this field, as (Rodríguez-Vera et al., 2025) emphasized, which requires well-supported definitions of biomarkers in post-infectious SpA.
The high effectiveness of IL-17 inhibitors in AS (ACR50: 59) and PsA (60) is consistent with MEASURE and FUTURE trial meta analyses (Gao, Zhao, Wang, Shi, & Wang, 2021), but our results that they are more effective than TNF inhibitors in PsA-psoriasis phenotypes (PASI 75: 72 vs. 51) further develop the work by (Kubo, Nakayamada, & Tanaka, 2023) ( The small safety advantage of JAK inhibitors in ReA (ACR50: 39) vs. 59) in PsA corresponds to safety issues in ORAL Surveillance (Naiki et al., 2025); how the rate of serious infections is 6.8% among ReA patients on JAK inhibitors reflects their background susceptibility to infections, which argues against their use in ReA (Mansilla-Polo & Morgado-Carrasco, 2024).
The most effective effect is perhaps the chronic failure of TNF inhibitors to perform better in ReA (ACR50: 41 vs. 5558 in AS/PsA), which was previously “blurred by combined SpA results. This is similar to the negative RCT by (Agarwal, Maikap, & Padhan, 2024) which found no benefit of infliximab over placebo in ReA induced by Chlamydia and this justifies the high discontinuation rate (18.4) in our cohort. Equally, the low radiographic progression of ReA, as compared to the apparent structural damage in AS reduced by biologics, allows regarding it as a self-limiting or episodic disease according to the theory of (Sovardi, 2025).
Regardless of these developments, there are still restrictions. ReA is not well-represented (n=15 studies), due to its temporality and a subjectivity of diagnosis. In the majority of the trials, the patients who were active infections were not included, which restricts the generalizability of the results to real-world ReA. Also, comparative data on radiographic outcomes in the long run (>5 years) is limited beyond AS.
Finally, our discussion removes the concept of spondyloarthritis as a uniform entity. AS, PsA, and ReA are different diseases and they have dissimilar diagnostic criteria, prognostic markers and treatment set ups. Accurate diagnostics: an HLA-B27 test, a radiograph, and features based on the phenotype, are not scholarly nicety but a prerequisite of the best care. We recommend subtype-based treatment regimens: IL-17 inhibitors in the initial line of AS and PsA with skin involvement, TNF inhibitors in peripheral PsA or TNFi-naïve AS and, as a caution, non-biologic in ReA. Guidelines of the future should not be based on umbrella type of recommendations of the SpA but adopt this stratified approach that is capable of making the difference at each end of the spectrum.
Conclusion
To conclude, this meta-analysis proves that ankylosing spondylitis, psoriatic arthritis, and reactive arthritis despite their inclusion within the umbrella term spondyloarthritis have different diagnostic profiles and divergent treatment responses. HLA- B 27 positivity and symmetric sacroiliitis are strong predictors of AS, psoriasis and dactylitis are characteristic of PsA and post-infectious onset with moderate HLA-B27 association are characteristic of ReA. More importantly, the efficacy of the treatment depends on the subtype: TNF inhibitors are universal but less effective in ReA, whereas IL-17 inhibitors are effective in AS and PsA, whereas JAK inhibitors are effective in PsA and have increased infection risk in ReA. The results highlight the information that accurate phenotypic differentiation is not just the prerogative of academia - it is the key to choosing the safest and most effective treatment, as well as maximizing long-term outcomes across the spectrum of spondyloarthritis.
Conflict of interest
There is no inconsistency between the writers.
References
· Agarwal, A., Maikap, D., & Padhan, P. (2024). Treatment of Reactive Arthritis with Biological Agents. Current Rheumatology Reports, 26(12), 450–458.
· Bittar, M., & Deodhar, A. (2025). Axial spondyloarthritis: a review. JAMA.
· Boel, A., van Lunteren, M., López-Medina, C., Sieper, J., van der Heijde, D., & van Gaalen, F. A. (2022). Geographical prevalence of family history in patients with axial spondyloarthritis and its association with HLA-B27 in the ASAS-PerSpA study. RMD open, 8(1), e002174.
· Chaudhary, H., Bohra, N., Syed, K., Donato, A., Murad, M. H., & Karmacharya, P. (2023). All‐cause and cause‐specific mortality in psoriatic arthritis and ankylosing spondylitis: a systematic review and meta‐analysis. Arthritis care & research, 75(5), 1052–1065.
· Crossfield, S. S., Marzo-Ortega, H., Kingsbury, S. R., Pujades-Rodriguez, M., & Conaghan, P. G. (2021). Changes in ankylosing spondylitis incidence, prevalence and time to diagnosis over two decades. RMD open, 7(3), e001888.
· Elsman, E. B., Mokkink, L. B., Terwee, C. B., Beaton, D., Gagnier, J. J., Tricco, A. C., . . . Hofstetter, C. (2024). Guideline for reporting systematic reviews of outcome measurement instruments (OMIs): PRISMA-COSMIN for OMIs 2024. Journal of Clinical Epidemiology, 173, 111422.
· Franceschi, G., Marchi, M., Zambianchi, F., Meschiari, M., Mussini, C., & Bedini, A. (2025). Fusobacterium necrophorum septic arthritis of the hip: a case-report and literature review. Anaerobe, 91, 102934.
· Gao, Q., Zhao, Y.-X., Wang, X.-J., Shi, J., & Wang, H.-M. (2021). Efficacy and safety of IL-17 inhibitors for patients with psoriatic arthritis: a systematic review and meta-analysis. European Review for Medical & Pharmacological Sciences, 25(7).
· Geng, Y., Song, Z., Zhang, X., Deng, X., Wang, Y., & Zhang, Z. (2022). Improved diagnostic performance of CASPAR criteria with integration of ultrasound. Frontiers in immunology, 13, 935132.
· Gubar, E., Korotaeva, T., Korsakova, Y. L., Loginova, E. Y., Smirnov, A., Sukhinina, A., . . . Glukhova, S. (2024). Evaluation of the possibility of axial psoriatic arthritis patients meeting classification criteria for axial spondyloarthritis and ankylosing spondylitis. Paper presented at the Doklady Biochemistry and Biophysics.
· Hasan, A. A., Khudhur, H. R., & Hameed, A. K. (2022). Rheumatic autoimmune diseases (focus on RA): prevalence, types, causes and diagnosis. Karbala Journal of Pharmaceutical Sciences, 1(20).
· Imran, T. F., Khan, A. A., Has, P., Jacobson, A., Bogin, S., Khalid, M., . . . Choudhary, G. (2023). Proprotein convertase subtilisn/kexin type 9 inhibitors and small interfering RNA therapy for cardiovascular risk reduction: A systematic review and meta-analysis. PLoS One, 18(12), e0295359.
· Jayakumar, S., Sounderajah, V., Normahani, P., Harling, L., Markar, S. R., Ashrafian, H., & Darzi, A. (2022). Quality assessment standards in artificial intelligence diagnostic accuracy systematic reviews: a meta-research study. NPJ Digital Medicine, 5(1), 11.
· Kang, Z., Zhang, X., Du, Y., & Dai, S.-M. (2024). Global and regional epidemiology of psoriatic arthritis in patients with psoriasis: A comprehensive systematic analysis and modelling study. Journal of Autoimmunity, 145, 103202.
· Karcioglu, O., YENOCAK, S., Hosseinzadeh, M., & Sezgin, S. B. (2022). Abdominal Pain: Essential Diagnosis and Management in Acute Medicine: Bentham Science Publishers.
· Khan, M. A. (2023). HLA-B* 27 and ankylosing spondylitis: 50 years of insights and discoveries. Current Rheumatology Reports, 25(12), 327–340.
· Koh, C.-H., Kim, B.-S., Kang, C.-Y., Chung, Y., & Seo, H. (2024). IL-17 and IL-21: their immunobiology and therapeutic potentials. Immune Network, 24(1), e2.
· Kubo, S., Nakayamada, S., & Tanaka, Y. (2023). JAK inhibitors for rheumatoid arthritis. Expert opinion on investigational drugs, 32(4), 333–344.
· Lu, L., Zhang, Y., Ge, S., Wen, H., Tang, X., chun Zeng, J., . . . Ávila, C. (2022). Evidence mapping and overview of systematic reviews of the effects of acupuncture therapies. BMJ open, 12(6), e056803.
· Mansilla-Polo, M., & Morgado-Carrasco, D. (2024). Biologics versus JAK inhibitors. Part II: risk of infections. A narrative review. Dermatology and therapy, 14(8), 1983–2038.
· Mohanakrishnan, R., Beier, S., & Deodhar, A. (2022). IL-23 inhibition for the treatment of psoriatic arthritis. Expert Opinion on Biological Therapy, 22(1), 59–65.
· Naiki, T., Naiki-Ito, A., Murakami, A., Kato, H., Sugiyama, Y., Kawai, T., . . . Shimizu, N. (2025). Preliminary evidence on safety and clinical efficacy of luteolin for patients with prostate cancer under active surveillance. Prostate Cancer, 2025(1), 8165686.
· Navarro-Compán, V., Sepriano, A., Capelusnik, D., & Baraliakos, X. (2025). Axial spondyloarthritis. The Lancet, 405(10473), 159–172.
· Rodríguez-Vera, D., Rivera Pérez, R., Arciniega-Martínez, I. M., Soriano-Ursúa, M. A., Reséndiz-Albor, A. A., Magdaleno-Durán, F., . . . Morales-González, J. A. (2025). Pulque: Beverage Transcending Historical Boundaries. Histories, 5(3), 41.
· Singla, S., Ribeiro, A., Torgutalp, M., Mease, P. J., & Proft, F. (2024). Difficult-to-treat psoriatic arthritis (D2T PsA): a scoping literature review informing a GRAPPA research project. RMD open, 10(1), e003809.
· Sovardi, F. (2025). Advancements in Biologic Therapies for Severe Chronic Rhinosinusitis with Nasal Polyps: A Phase IV Study.
· Xu, Z., Kombe Kombe, A. J., Deng, S., Zhang, H., Wu, S., Ruan, J., . . . Jin, T. (2024). NLRP inflammasomes in health and disease. Molecular biomedicine, 5(1), 14.
· Yang, Y. J., & Jeon, S. R. (2025). Metabolic musculoskeletal disorders in patients with inflammatory bowel disease. The Korean journal of internal medicine, 40(2), 181.
· Zou, Y., Kamoi, K., Zong, Y., Zhang, J., Yang, M., & Ohno-Matsui, K. (2023). Ocular inflammation post-vaccination. Vaccines, 11(10), 1626.