Diseases of the Sexual Gland in Children
1. Megha Hariraj
2. Gulnaz Osmonova
(1. Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.
2. Teacher, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.)
Abstract
Diseases of the sexual glands in children represent an important group of endocrine disorders that significantly influence growth, pubertal development, reproductive potential, and psychosocial well-being. Normal sexual maturation is regulated by the hypothalamic–pituitary–gonadal (HPG) axis, and disturbances at any level of this axis can result in abnormal timing or progression of puberty. These disorders may manifest as premature sexual development (precocious puberty), hypogonadism, or delayed sexual development. Each condition has diverse etiological factors ranging from constitutional and functional variations to genetic, endocrine, neoplastic, and central nervous system pathologies. Early recognition and accurate diagnosis are essential to prevent long-term complications such as compromised adult height, infertility, metabolic disturbances, and psychological distress.
This article provides a comprehensive review of diseases of the sexual glands in children, focusing on the etiopathogenesis, clinical manifestations, and diagnostic evaluation of premature sexual development, hypogonadism, and delayed sexual development.
Emphasis is placed on understanding the underlying pathophysiology, recognizing key clinical patterns, and applying a structured diagnostic approach suitable for pediatric and adolescent populations.
Introduction
Sexual development in children is a complex, finely regulated biological process that marks the transition from childhood to sexual maturity. The sexual glands—testes in males and ovaries in females—play a central role in this process by producing sex steroids and gametes under the control of the hypothalamic–pituitary–gonadal (HPG) axis. Normal pubertal development follows a predictable sequence and timing; however, deviations from this pattern may indicate underlying pathology.
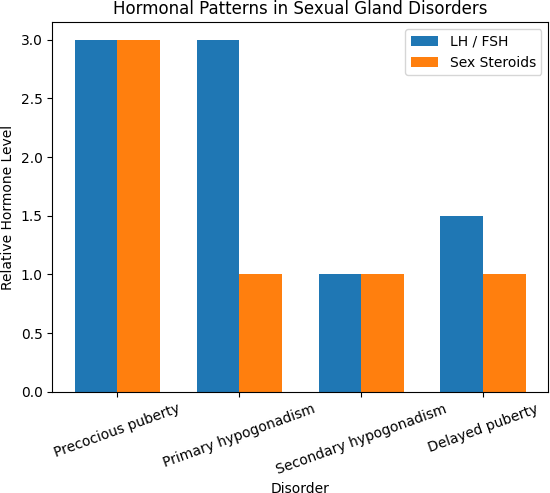
Diseases of the sexual glands in children can broadly present in three major clinical patterns: premature sexual development, hypogonadism, and delayed sexual development. Premature activation of the gonads results in early onset of secondary sexual characteristics, while inadequate gonadal function leads to absent or incomplete sexual maturation. Delayed sexual development may represent a benign constitutional variant or may be a manifestation of chronic disease or endocrine dysfunction.
These conditions are of particular clinical importance because their effects extend beyond physical development to include final adult height, fertility potential, bone health, metabolic status, and psychosocial development. In addition, early or delayed puberty often causes significant emotional stress for both the child and family. Advances in pediatric endocrinology, molecular genetics, and imaging techniques have improved diagnostic accuracy and enhanced understanding of the etiopathogenesis of these disorders.
This article aims to systematically review diseases of the sexual glands in children, with a focused discussion on premature sexual development, hypogonadism, and delayed sexual development. The etiological factors, pathophysiological mechanisms, clinical features, and diagnostic strategies are described in detail to provide a clear framework for academic learning and clinical application.
Normal Physiology of Sexual Gland Development
Understanding disorders of sexual gland function requires a clear knowledge of normal pubertal physiology.
1.1 Hypothalamic–Pituitary–Gonadal (HPG) Axis
Puberty is initiated and regulated by the HPG axis:
● The hypothalamus secretes gonadotropin-releasing hormone (GnRH) in a pulsatile manner.
● GnRH stimulates the anterior pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
● LH and FSH act on the gonads, stimulating the production of sex steroids (testosterone in males, estrogen and progesterone in females) and gametogenesis.
During childhood, the HPG axis is physiologically suppressed. At puberty, reactivation of pulsatile GnRH secretion leads to progressive sexual maturation.
1.2 Sexual Gland Function
● Testes: Produce testosterone and spermatozoa; responsible for male secondary sexual characteristics, growth of external genitalia, and spermatogenesis.
● Ovaries: Produce estrogen and progesterone; regulate breast development, menstrual cycle, and ovulation.
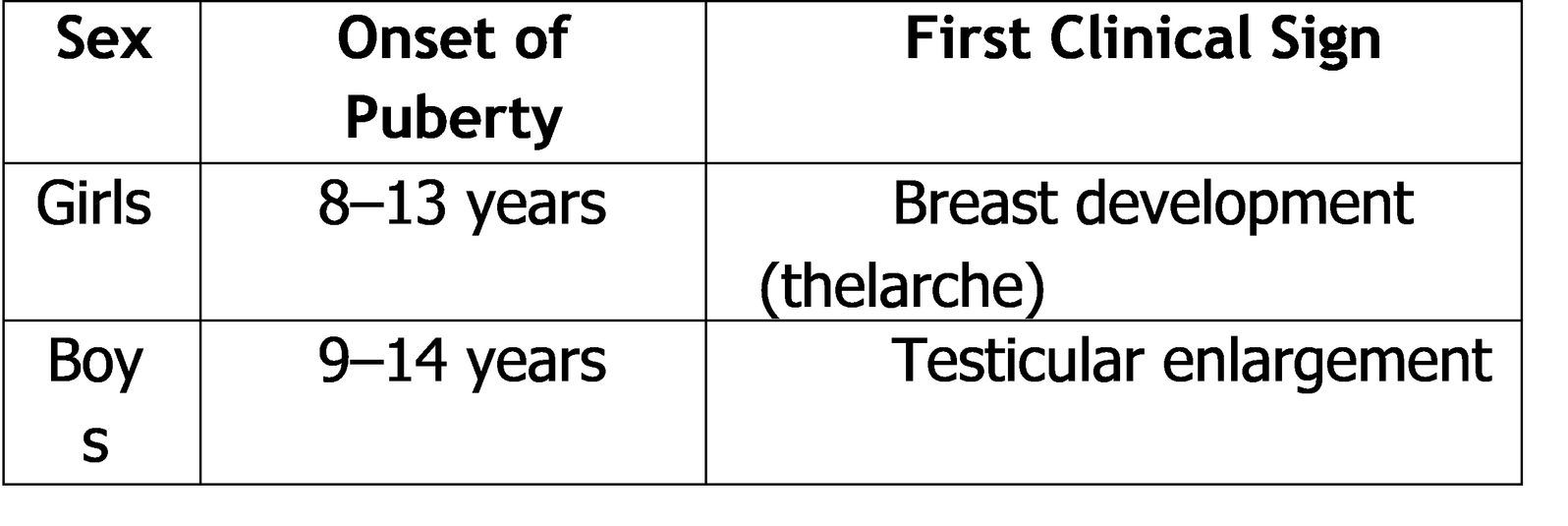
1.3 Normal Timing of Puberty
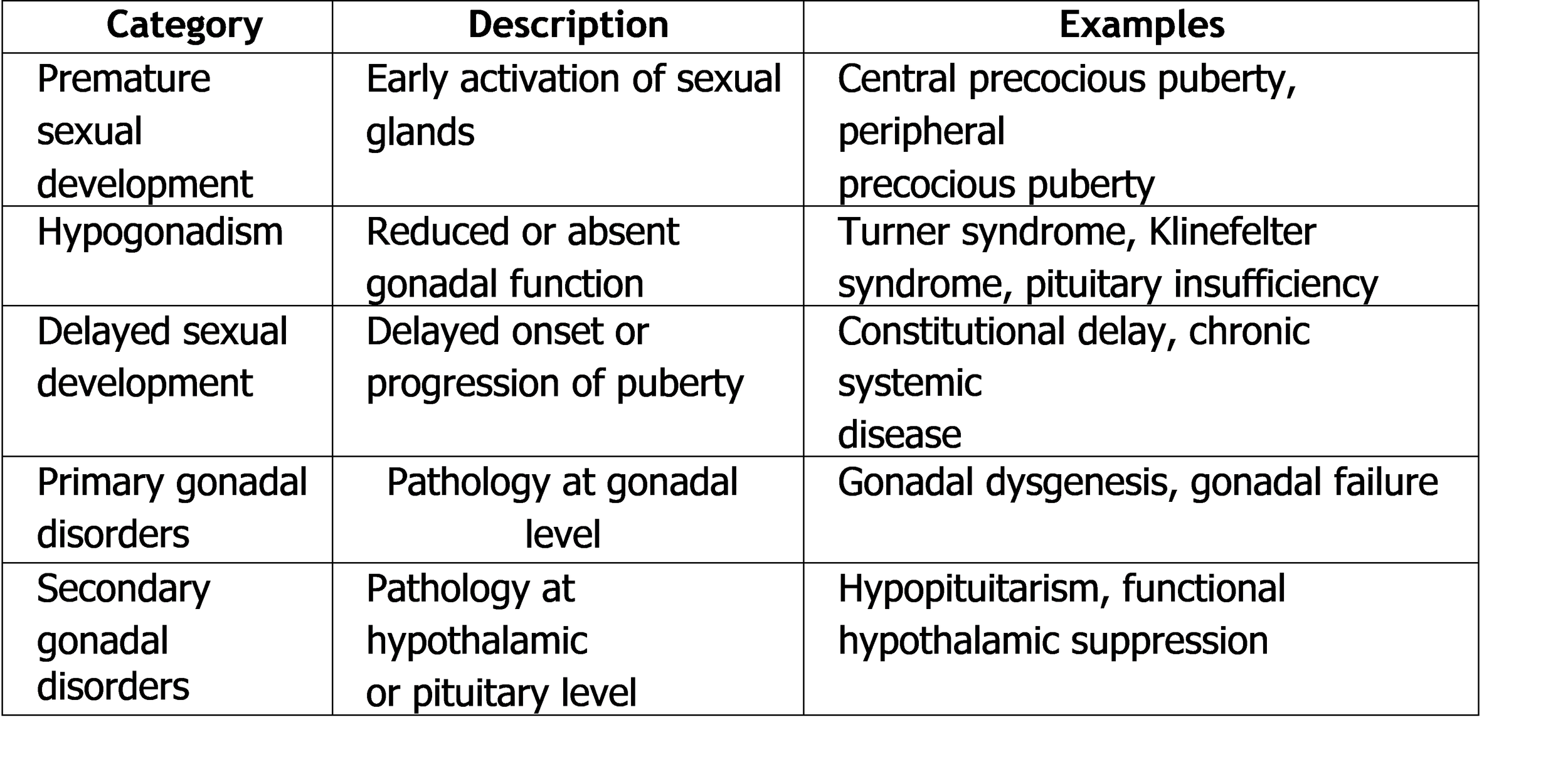
Classification of Diseases of the Sexual Glands in Children
Sexual gland disorders in children can be classified based on the timing of pubertal development and the level of dysfunction within the HPG axis.
Table 1. Classification of Diseases of the Sexual Glands in Children
1.4 Basis of Classification
● Chronological: Early, normal, or delayed puberty
● Anatomical: Hypothalamic, pituitary, or gonadal origin
● Functional: Hormone excess or deficiency
This classification aids in narrowing differential diagnoses and guiding diagnostic evaluation.
2. Overview of Major Sexual Gland Disorders in Children
● Premature sexual development results from early exposure to sex steroids and may be GnRH-dependent or independent.
● Hypogonadism refers to insufficient production of sex steroids and/or gametes and may be primary or secondary.
● Delayed sexual development is characterized by failure to initiate or complete puberty at the expected age.
Each of these conditions has distinct etiological mechanisms, clinical manifestations, and diagnostic criteria, which will be discussed in detail in subsequent sections.
3. Premature Sexual Development (Precocious Puberty)
3.1 Definition
Premature sexual development, commonly referred to as precocious puberty, is defined as the onset of secondary sexual characteristics before the normal age of pubertal onset:
● Girls: Before 8 years of age
● Boys: Before 9 years of age
It results from early activation of the hypothalamic–pituitary–gonadal (HPG) axis or from excess sex steroid production independent of gonadotropin stimulation.
Precocious puberty is clinically significant because it may lead to:
● Accelerated linear growth with premature epiphyseal closure
● Reduced final adult height
● Early psychosocial stress
● Underlying serious pathology, especially in boys
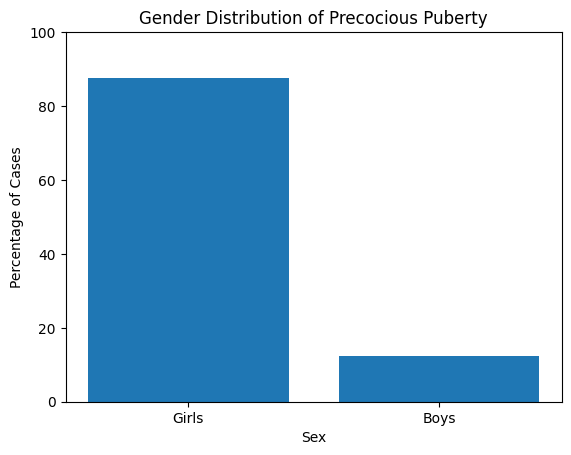
3.2 Epidemiology
● Precocious puberty is more common in girls than boys (female-to-male ratio ≈
10:1).
● The majority of cases in girls are idiopathic, whereas boys have a higher likelihood of identifiable organic pathology.
● The reported incidence has increased globally, partly due to:
o Improved recognition
o Environmental influences
o Rising childhood obesity
Graph 1. Gender Distribution of Precocious Puberty
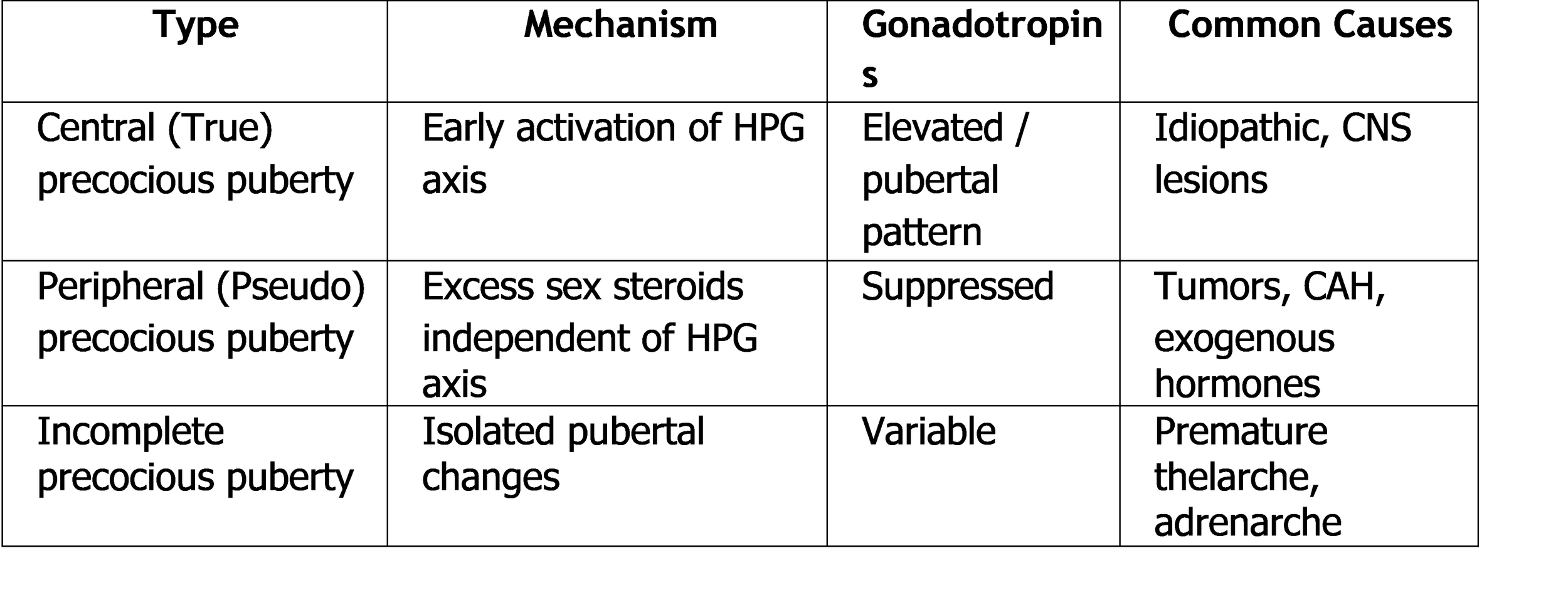
Classification of Precocious Puberty
Precocious puberty is broadly classified into central (gonadotropin-dependent) and
peripheral (gonadotropin-independent) forms.
Table 2. Classification of Precocious Puberty
4. Etiopathogenesis of Premature Sexual Development
4.1 Central Precocious Puberty (CPP)
Central precocious puberty results from premature maturation of the HPG axis, leading to pulsatile GnRH secretion and subsequent gonadotropin release.
Etiological Factors
● Idiopathic (most common in girls)
● Central nervous system lesions, including:
o Hypothalamic hamartoma
o Brain tumors (astrocytoma, glioma)
o Hydrocephalus
o CNS infections or trauma
● Genetic mutations
o MKRN3 gene mutations
o KISS1/KISS1R pathway abnormalities
Pathogenesis
● Early GnRH pulsatility → ↑ LH and FSH
● Gonadal stimulation → ↑ estrogen or testosterone
● Progressive pubertal development following normal pubertal sequence, but at an abnormally early age
4.2 Peripheral Precocious Puberty
Peripheral precocious puberty occurs due to sex steroid excess independent of pituitary gonadotropins.
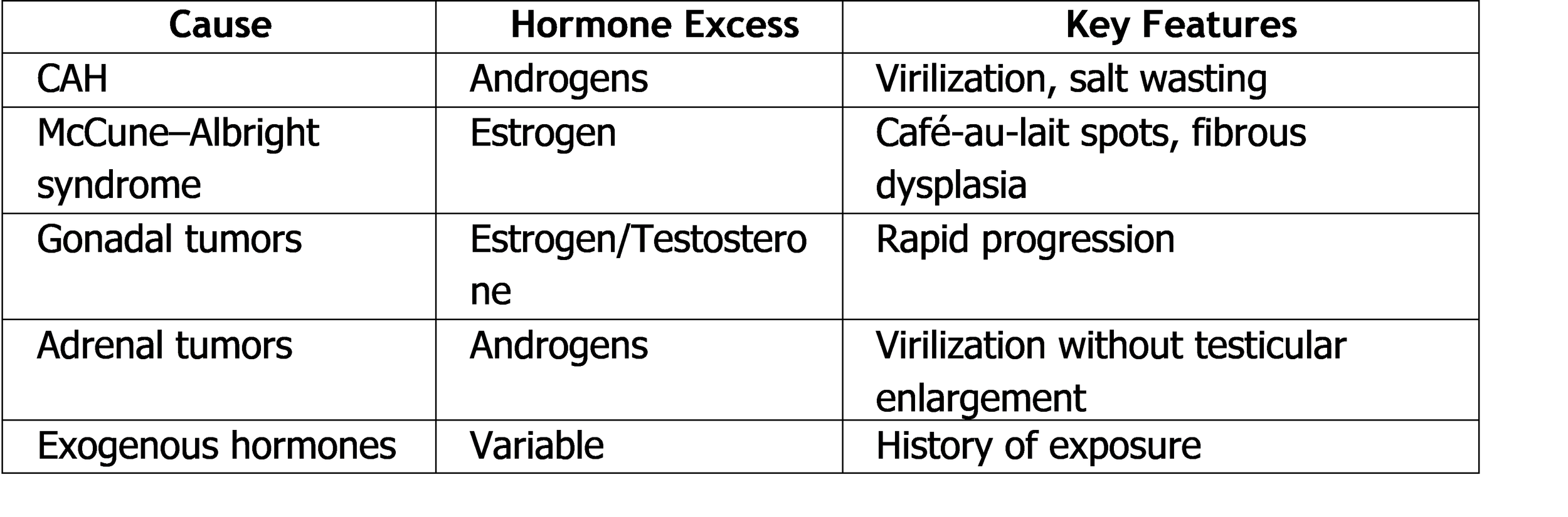
Etiological Factors
● Congenital adrenal hyperplasia (CAH)
● Gonadal tumors (Leydig cell tumors, ovarian tumors)
● Adrenal tumors
● McCune–Albright syndrome
● Exogenous exposure to sex steroids
Pathogenesis
● Autonomous production of sex steroids
● Suppression of LH and FSH due to negative feedback
● Pubertal changes may be incomplete or atypical
Table 3. Etiology of Peripheral Precocious Puberty
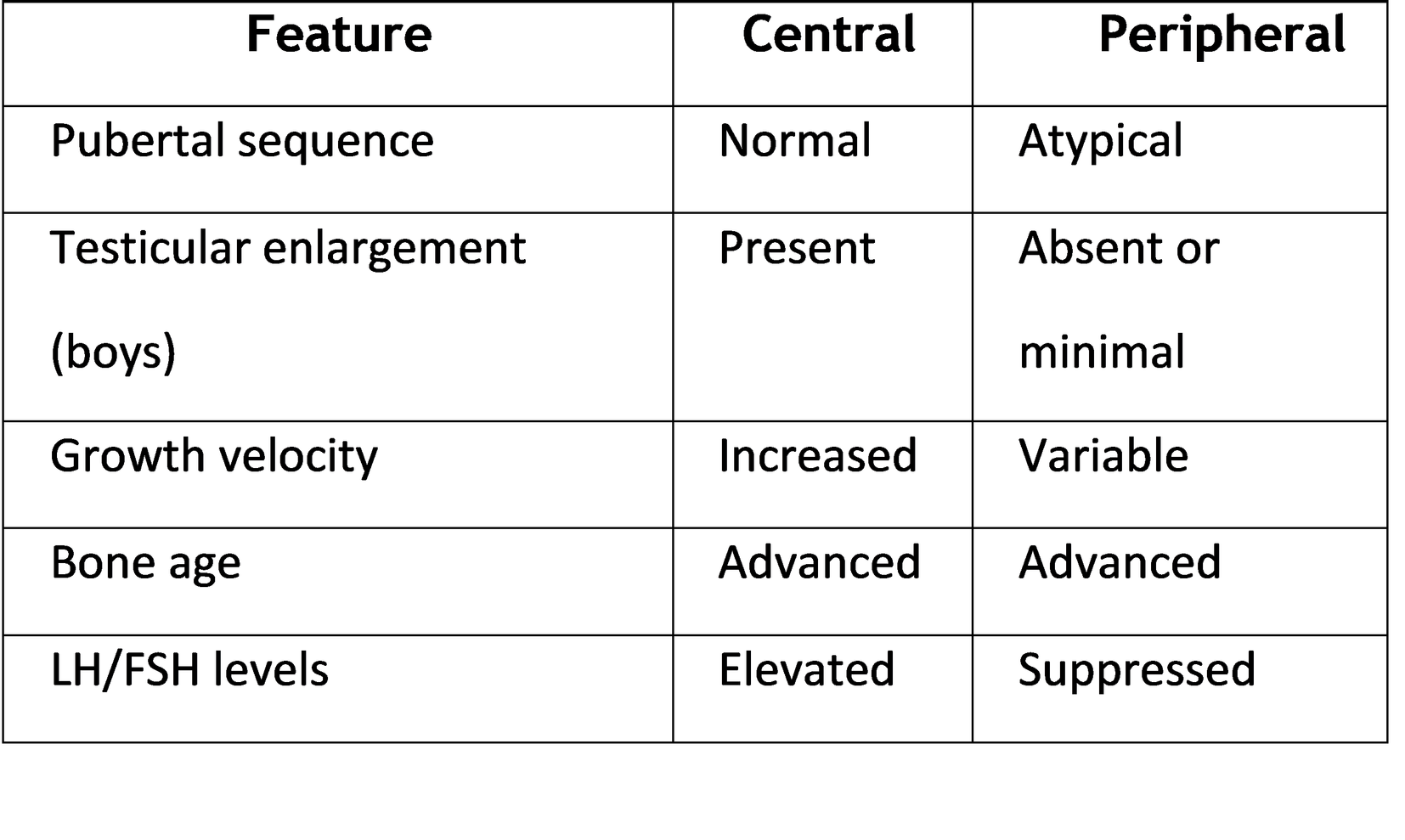
5. Clinical Features of Precocious Puberty
5.1 General Features
● Early development of secondary sexual characteristics
● Accelerated growth velocity
● Advanced bone age
● Emotional and behavioral changes
5.2 Clinical Features in Girls
● Breast development (thelarche)
● Pubic and axillary hair
● Menarche (in advanced cases)
● Estrogenized vaginal mucosa
5.3 Clinical Features in Boys
● Testicular enlargement (central type)
● Penile enlargement
● Pubic hair development
● Deepening of voice
● Increased muscle mass
Table 4. Comparison of Clinical Features in Central vs Peripheral Precocious Puberty
6. Diagnostic Evaluation of Precocious Puberty
A stepwise diagnostic approach is essential to determine the underlying cause.
6.1 Clinical Assessment
● Detailed history (onset, progression, exposure to hormones)
● Growth chart analysis
● Tanner staging
● Neurological examination
6.2 Laboratory Investigations
● Basal LH and FSH
● Sex steroid levels (estradiol/testosterone)
● GnRH stimulation test (gold standard)
● Serum 17-hydroxyprogesterone (if CAH suspected)
● Thyroid function tests
6.3 Imaging Studies
● Bone age assessment (left hand and wrist X-ray)
● Pelvic ultrasound (girls)
● Testicular ultrasound (boys)
● MRI brain (mandatory in boys and young girls)
G. Summary of Key Points
● Precocious puberty is defined by early activation of pubertal changes
● Central precocious puberty is GnRH-dependent and often idiopathic in girls
● Peripheral precocious puberty is due to autonomous hormone secretion
● Accurate differentiation is essential for appropriate management
● Early diagnosis prevents long-term complications
10. Hypogonadism in Children
10.1 Definition
Hypogonadism in children is a clinical condition characterized by insufficient production of sex hormones and/or impaired gametogenesis due to dysfunction of the sexual glands (testes or ovaries) or their regulatory mechanisms. The disorder may present in
infancy, childhood, or adolescence, depending on the timing and severity of hormonal deficiency.
Hypogonadism interferes with:
● Normal pubertal development
● Secondary sexual characteristic formation
● Linear growth and bone mineralization
● Fertility potential
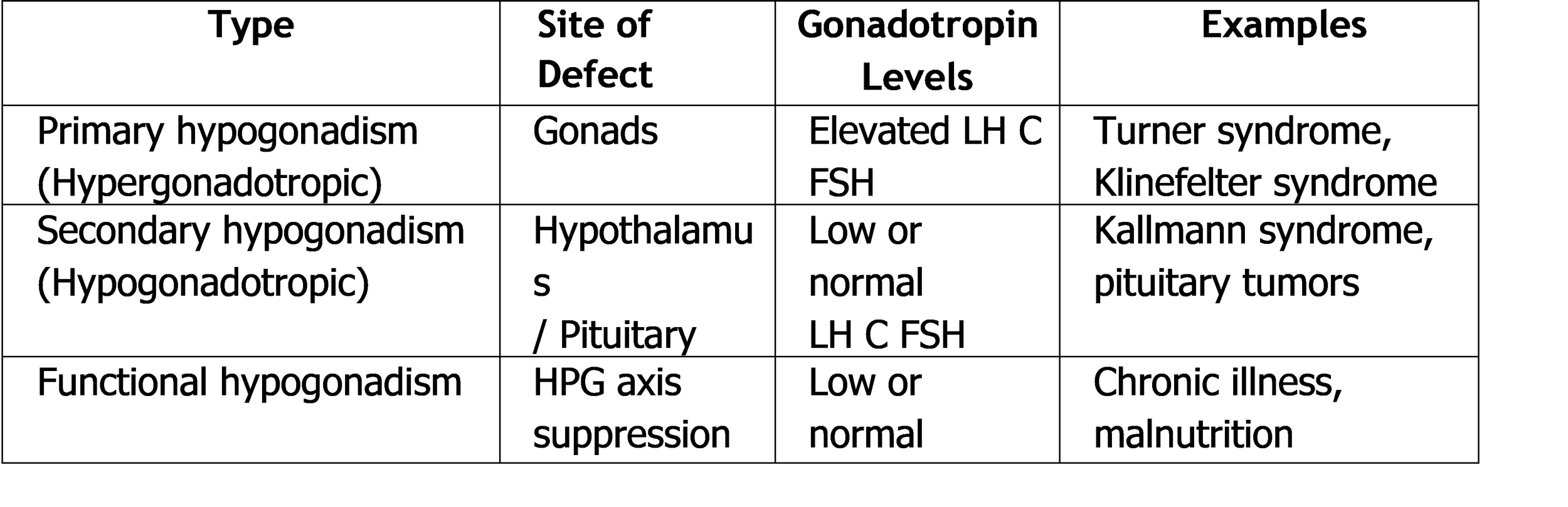
10.2 Classification of Hypogonadism
Hypogonadism is classified based on the level of dysfunction within the HPG axis.
Table 5. Classification of Hypogonadism in Children
11. Etiopathogenesis of Hypogonadism
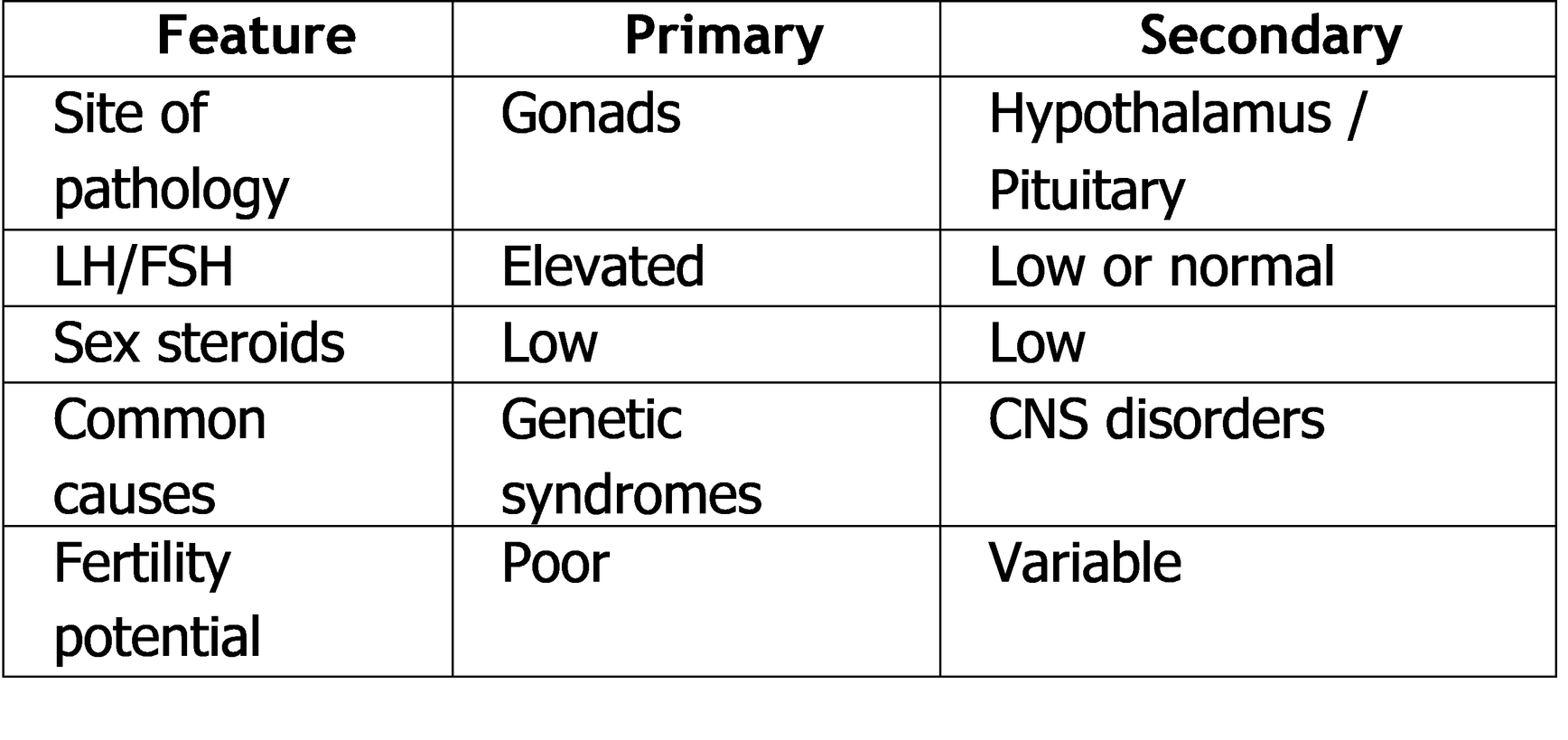
11.1 Primary Hypogonadism (Hypergonadotropic Hypogonadism)
Primary hypogonadism results from intrinsic gonadal failure, leading to inadequate sex steroid production despite increased gonadotropin stimulation.
Etiological Factors
● Genetic disorders
o Turner syndrome (45,XO)
o Klinefelter syndrome (47,XXY)
o Gonadal dysgenesis
● Congenital absence or damage
o Anorchia
o Ovarian agenesis
● Acquired causes
o Gonadal torsion
o Chemotherapy or radiotherapy
o Autoimmune gonadal destruction
o Infections (e.g., mumps orchitis)
Pathogenesis
● Gonadal failure → ↓ sex steroids
● Loss of negative feedback → ↑ LH and FSH
● Failure of pubertal progression
11.2 Secondary Hypogonadism (Hypogonadotropic Hypogonadism)
Secondary hypogonadism arises from deficient GnRH or gonadotropin secretion, resulting in reduced stimulation of otherwise normal gonads.
Etiological Factors
● Congenital
o Kallmann syndrome (GnRH deficiency with anosmia)
o Congenital hypopituitarism
● Acquired
o Pituitary adenomas
o Craniopharyngioma
o CNS infections or trauma
● Functional
o Chronic systemic illness
o Severe malnutrition
o Excessive physical stress
Pathogenesis
● ↓ GnRH secretion → ↓ LH and FSH
● Reduced gonadal stimulation
● Delayed or absent pubertal development
Table 6. Etiological Comparison of Primary and Secondary Hypogonadism
12. Clinical Features of Hypogonadism
Clinical manifestations depend on the age of onset and severity of hormonal deficiency.
12.1 Infancy
● Micropenis (boys)
● Cryptorchidism
● Ambiguous genitalia (in severe cases)
12.2 Childhood
● Usually asymptomatic
● Failure to initiate pubertal changes at expected age
12.3 Adolescence
● Delayed or absent secondary sexual characteristics
● Poor growth spurt
● Eunuchoid body proportions
● Sparse body hair
● Lack of breast development (girls)
● Small testes and penis (boys)
13. Diagnostic Evaluation of Hypogonadism
13.1 Clinical Assessment
● Detailed growth and pubertal history
● Tanner staging
● Family history of delayed puberty or infertility
13.2 Laboratory Investigations
● Serum LH and FSH
● Sex steroid levels (testosterone, estradiol)
● Prolactin levels
● Thyroid function tests
● Cortisol (if pituitary disease suspected)
13.3 Imaging Studies
● Bone age assessment
● Pelvic ultrasound (girls)
● Testicular ultrasound (boys)
● MRI of hypothalamic–pituitary region
13.4 Genetic Testing
● Karyotype analysis
● Targeted gene testing (when indicated)
14. Summary of Key Points
● Hypogonadism may be primary or secondary
● Genetic syndromes are common causes in children
● Clinical presentation varies with age
● Hormonal evaluation is central to diagnosis
● Early diagnosis improves long-term outcomes
15. Delayed Sexual Development (Delayed Puberty)
15.1 Definition
Delayed sexual development, also known as delayed puberty, is defined as the absence of initiation or progression of pubertal development beyond the expected age range.
Diagnostic age thresholds:
● Girls: Absence of breast development by 13 years or absence of menarche by 15– 16 years
● Boys: Absence of testicular enlargement by 14 years
Delayed puberty may represent a normal physiological variation or may indicate underlying endocrine or systemic pathology.
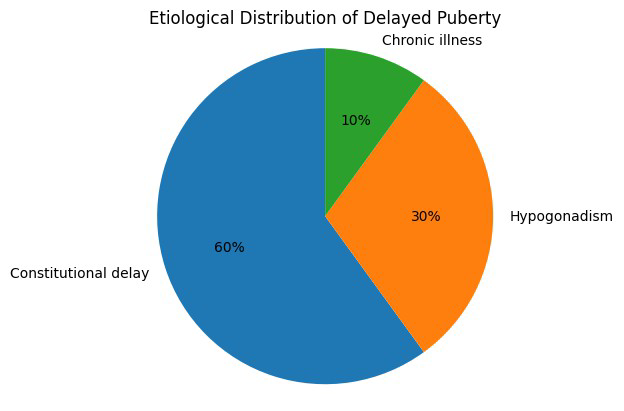
15.2 Epidemiology
● Delayed puberty affects approximately 2–3% of adolescents.
● More common in boys than girls.
● Constitutional delay of growth and puberty (CDGP) is the most frequent cause.
● Pathological causes must always be excluded before labeling a child as having CDGP.
Graph 2. Distribution of Causes of Delayed Puberty
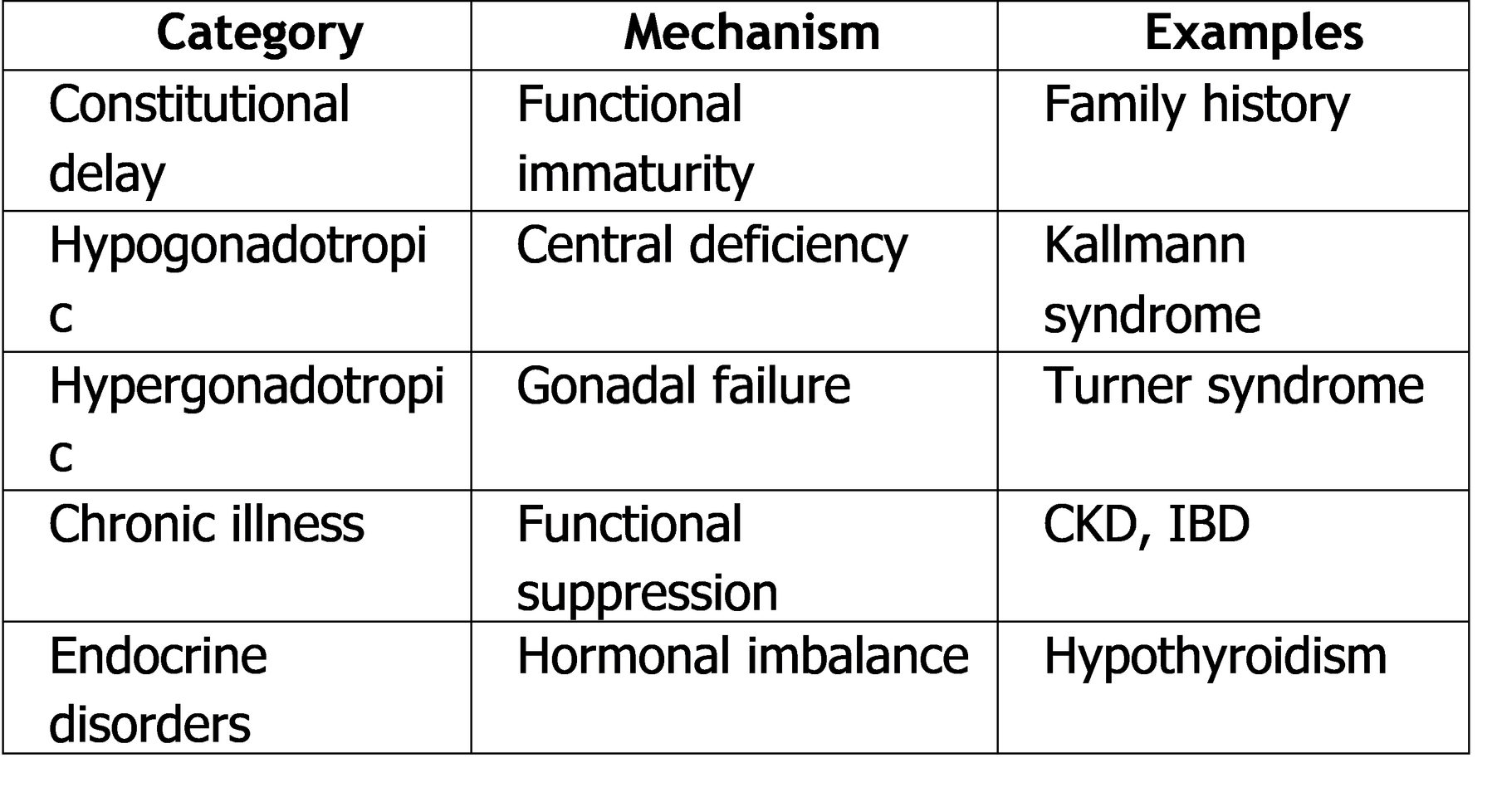
16. Etiopathogenesis of Delayed Sexual Development
Delayed sexual development occurs due to failure or delay in activation of the HPG axis
or due to reduced responsiveness of the gonads.
16.1 Constitutional Delay of Growth and Puberty (CDGP)
CDGP is a benign, self-limiting condition characterized by delayed skeletal maturation and delayed pubertal onset.
Etiological Factors
● Familial pattern
● Delayed maturation of GnRH pulsatility
Pathogenesis
● Temporary immaturity of the HPG axis
● Normal progression of puberty occurs later than peers
16.2 Hypogonadotropic Hypogonadism
● Due to deficient GnRH or gonadotropin secretion
● May be congenital or acquired Common causes:
● Kallmann syndrome
● Pituitary tumors
● Chronic systemic diseases
16.3 Hypergonadotropic Hypogonadism
● Primary gonadal failure
● Gonads fail to respond to gonadotropins Common causes:
● Turner syndrome
● Klinefelter syndrome
● Gonadal damage due to chemotherapy
Table 8. Etiological Classification of Delayed Sexual Development
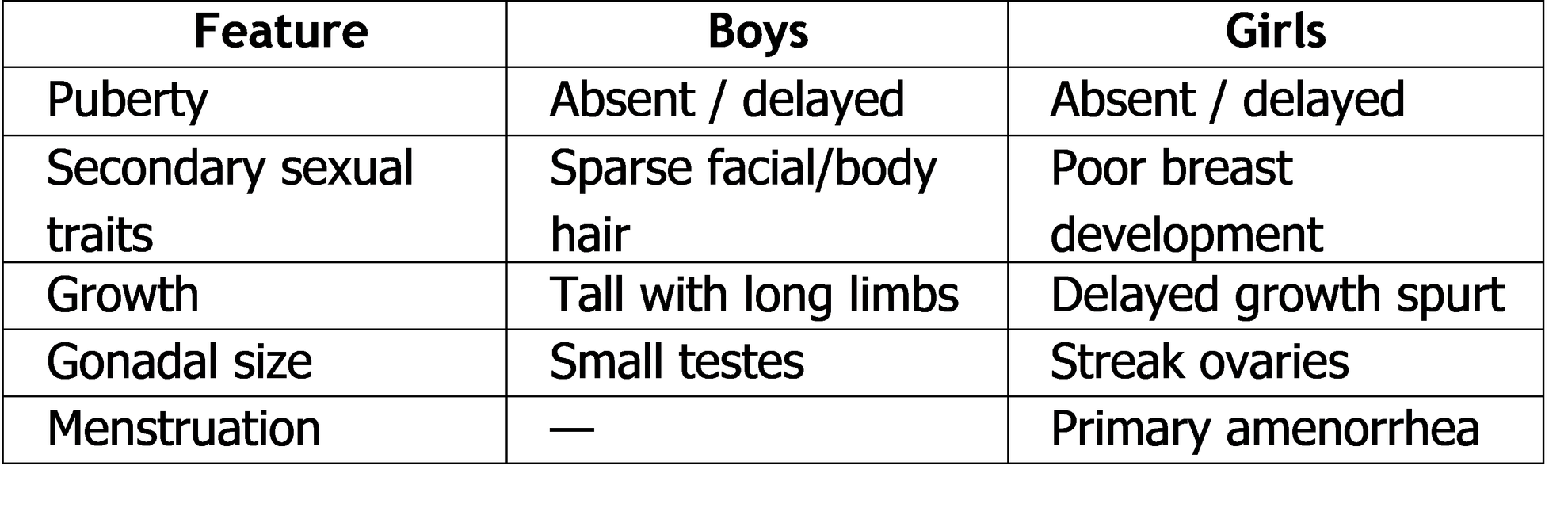
17. Clinical Features of Delayed Sexual Development
17.1 General Features
● Short stature compared to peers
● Delayed growth spurt
● Immature appearance
17.2 Clinical Features in Boys
● Small testes (<4 mL)
● Absence of pubic hair
● Lack of voice deepening
● Eunuchoid body proportions (in long-standing cases)
17.3 Clinical Features in Girls
● Absence of breast development
● Primary amenorrhea
● Lack of pubic and axillary hair
18. Diagnostic Evaluation of Delayed Sexual Development
A systematic evaluation is required to differentiate CDGP from pathological causes.
18.1 Clinical Assessment
● Growth pattern analysis
● Tanner staging
● Family history of delayed puberty
● Nutritional and chronic illness assessment
18.2 Laboratory Investigations
● Serum LH and FSH
● Estradiol (girls) / Testosterone (boys)
● Thyroid function tests
● Prolactin levels
● Inflammatory markers if chronic disease suspected
Radiological Evaluation
● Bone age assessment (delayed in CDGP)
● Pelvic ultrasound (girls)
● MRI pituitary (if central cause suspected)
20. Summary of Key Points
● Delayed puberty is common in adolescents
● CDGP is the most frequent cause
● Pathological causes must be excluded
● Hormonal evaluation is essential
● Early diagnosis prevents psychosocial distress
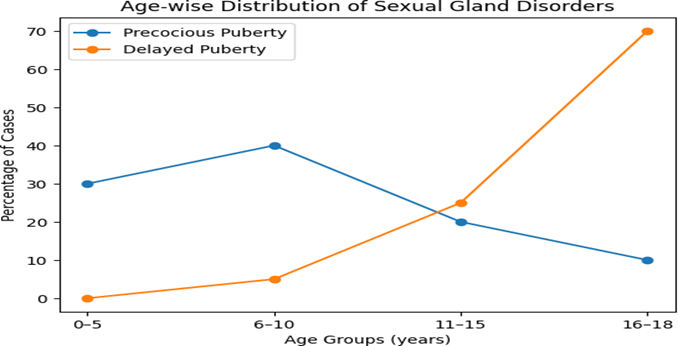
21. Comparative Overview of Sexual Gland Disorders in Children
A consolidated comparison of premature sexual development, hypogonadism, and delayed sexual development helps in rapid clinical differentiation and strengthens conceptual clarity.
Age-wise Distribution of Sexual Gland Disorders
23. Key Clinical Pearls
● Early pubertal signs always require evaluation, especially in boys.
● Bone age is a simple but powerful tool in assessing pubertal disorders.
● Hypogonadism should be suspected when puberty fails to progress despite age appropriateness.
● Constitutional delay is a diagnosis of exclusion.
● Psychological support is essential in children with abnormal pubertal timing.
24. Common Diagnostic Pitfalls
● Mistaking constitutional delay for permanent hypogonadism
● Delaying CNS imaging in boys with precocious puberty
● Ignoring subtle growth pattern abnormalities
● Failure to consider chronic systemic disease as a cause of delayed puberty
Conclusion
Diseases of the sexual glands in children constitute a diverse and clinically significant group of endocrine disorders that profoundly influence physical growth, sexual
maturation, reproductive potential, and psychosocial development. Premature sexual development, hypogonadism, and delayed sexual development represent distinct yet interrelated disturbances of the hypothalamic–pituitary–gonadal axis.
A clear understanding of normal pubertal physiology is essential for recognizing deviations and identifying underlying pathology. Etiological factors range from benign constitutional variations to serious genetic, endocrine, and central nervous system disorders. Early recognition and accurate diagnosis are critical in preventing long-term complications such as compromised adult height, infertility, metabolic disturbances, and psychological distress.
A structured diagnostic approach incorporating clinical assessment, hormonal evaluation, radiological imaging, and genetic studies allows precise differentiation between various disorders of sexual gland function. With timely intervention and appropriate follow-up, most affected children can achieve favorable health and developmental outcomes.
Continued advancements in pediatric endocrinology and increased awareness among clinicians will further improve the management and prognosis of these conditions.
References
1. Sperling MA. Pediatric Endocrinology. 5th ed. Philadelphia: Elsevier; 2020.
2. Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams Textbook of Endocrinology. 14th ed. Philadelphia: Elsevier; 2020.
3. Carel JC, Léger J. Precocious puberty. N Engl J Med. 2008;358:2366–77.
4. Palmert MR, Dunkel L. Delayed puberty. N Engl J Med. 2012;366:443–53.
5. Grumbach MM, Styne DM. Puberty: Ontogeny, neuroendocrinology, physiology, and disorders. In: Williams Textbook of Endocrinology.
6. Harrington J, Palmert MR. Clinical review: Differential diagnosis and management of delayed puberty. J Clin Endocrinol Metab. 2012;97:221–32.
7. Eugster EA. Hypogonadism in adolescents. Pediatr Clin North Am. 2011;58:1181– 200.