Endemic Goiter and Hypothyroidism in Children: A Public Health and Clinical Perspective
1. Gulnaz Osmonova
2. Mohd Hamid Ansari
(1. Teacher, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
(2. Students, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
Abstract
Endemic goiter and hypothyroidism remain significant public health problems in many developing regions. Children are particularly vulnerable due to increased iodine requirements for growth and neurodevelopment. This article reviews the epidemiology, pathophysiology, clinical features, prevention, and management strategies.
Endemic goiter and hypothyroidism in children represent significant yet preventable public health problems, particularly in regions with iodine-deficient soil and limited access to iodized salt. Adequate thyroid hormone levels are essential for normal physical growth, brain development, and metabolic regulation during childhood. Iodine deficiency leads to impaired synthesis of thyroid hormones, resulting in compensatory thyroid enlargement (goiter) and varying degrees of hypothyroidism. Children are especially vulnerable to the adverse effects of iodine deficiency, which may include growth retardation, delayed puberty, poor school performance, and irreversible neurocognitive impairment in severe cases.
From a clinical perspective, endemic goiter in children often presents as a painless enlargement of the thyroid gland, while hypothyroidism manifests with symptoms such as fatigue, cold intolerance, weight gain, constipation, dry skin, and delayed skeletal maturation. Diagnosis relies on clinical examination, biochemical assessment of thyroid function (serum TSH and thyroxine levels), urinary iodine concentration, and imaging studies when required. Early detection through school-based screening programs is crucial in endemic areas.
From a public health standpoint, endemic goiter and childhood hypothyroidism serve as key indicators of iodine deficiency disorders within a population. Universal salt iodization remains the most effective and cost-efficient preventive strategy worldwide. This article reviews the epidemiology, etiology, pathophysiology, clinical features, diagnostic approach, management, and prevention of endemic goiter and hypothyroidism in children, emphasizing the need for integrated clinical care and sustained public health interventions to eliminate iodine deficiency disorders and improve child health outcomes.
Keywords
Endemic goiter,Hypothyroidism in children, Iodine deficiency disorders (IDD), Pediatric thyroid disorders, Iodine deficiency, Universal salt iodization, Thyroid hormone deficiency, Child growth and development, Public health nutrition, Pediatric endocrinology, Goiter prevalence, Neurocognitive development, Preventable endocrine disorders.
Introduction
Endemic goiter is primarily caused by iodine deficiency, leading to thyroid enlargement and impaired thyroid hormone synthesis. In children, prolonged deficiency results in hypothyroidism, growth retardation, and cognitive impairment.
Endemic goiter and hypothyroidism in children represent significant yet preventable public health problems, particularly in regions where iodine deficiency remains prevalent. Iodine is an essential micronutrient required for the synthesis of thyroid hormones—thyroxine (T4) and triiodothyronine (T3)—which play a critical role in normal growth, neurodevelopment, and metabolic regulation. Inadequate iodine intake leads to impaired thyroid hormone production, resulting in compensatory enlargement of the thyroid gland (goiter) and varying degrees of hypothyroidism. Children are especially vulnerable to these effects due to their increased physiological demands for thyroid hormones during periods of rapid growth and brain development.
From a public health perspective, endemic goiter is considered a sensitive indicator of iodine deficiency in a population. The World Health Organization defines endemic goiter as a condition in which more than 5% of school-age children in a given area have an enlarged thyroid gland. Although substantial progress has been made globally through universal salt iodization programs, iodine deficiency disorders continue to affect millions of children, particularly in low- and middle-income countries, mountainous regions, and areas with iodine-depleted soil. These disorders contribute not only to visible thyroid enlargement but also to hidden consequences such as reduced intellectual capacity and impaired academic performance.
Clinically, hypothyroidism in children associated with iodine deficiency may present with subtle or overt manifestations, ranging from mild growth retardation and delayed puberty to severe neurocognitive impairment in cases of prolonged deficiency. Unlike adults, untreated hypothyroidism in children can result in irreversible damage, emphasizing the importance of early detection and timely intervention. School-based screening, biochemical assessment, and community surveillance play a vital role in identifying affected populations and individuals.
This article aims to provide a comprehensive overview of endemic goiter and hypothyroidism in children by integrating clinical knowledge with public health principles. It highlights the epidemiology, etiology, pathophysiology, clinical features, diagnostic approaches, management strategies, and preventive measures, with particular emphasis on iodine supplementation and health policy interventions. Understanding these aspects is essential for medical students, clinicians, and public health professionals working toward the elimination of iodine deficiency disorders and the promotion of optimal child health and development.
Epidemiology and Public Health Impact
1. Epidemiology
Endemic goiter is defined as a thyroid enlargement in a population where >5% of school-age children are affected. It is most commonly caused by iodine deficiency, though other factors such as selenium deficiency or goitrogenic foods can contribute.
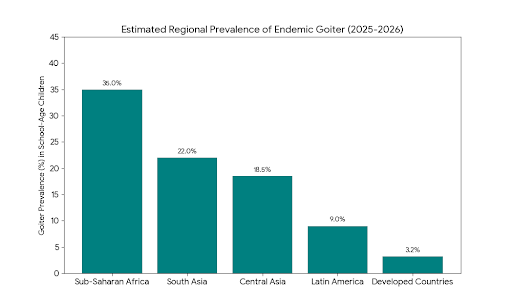
Global Prevalence
Worldwide, iodine deficiency affects over 2 billion people, with children being the most vulnerable.
School-age children are often the sentinel population in surveys.
Highest prevalence is in:
South Asia: India, Pakistan, Nepal
Sub-Saharan Africa: Ethiopia, Democratic Republic of Congo
Central Asia: Kyrgyzstan, Tajikistan
Developed countries have much lower prevalence due to universal salt iodization programs.
Trends
Universal salt iodization has reduced prevalence significantly in many regions.
Residual pockets remain in remote, mountainous, or rural areas with poor access to iodized salt.
Surveys often show:
Goiter prevalence: 3–40% depending on region
Iodine deficiency (<100 µg/L urinary iodine): common in school-age children
2. Public Health Impact
Endemic goiter and hypothyroidism in children are major public health problems because of their long-term developmental consequences:
A. Health Consequences
Physical Growth
Short stature and delayed skeletal maturation
Neurocognitive Development
Mild to severe mental retardation if hypothyroidism is untreated in early childhood
Poor school performance
Reproductive Health
Delayed puberty
Severe cases
Cretinism: irreversible mental and physical disability
B. Economic and Social Impact
Increased healthcare costs due to lifelong management
Reduced productivity and educational attainment
Burden on families and communities in endemic regions
C. Indicator of Public Health
Goiter prevalence in school-age children is used by WHO as an indicator of iodine deficiency in a population
Monitoring urinary iodine concentration (UIC) provides real-time assessment of iodine status
D. Preventive Significance
Effective public health interventions, particularly universal salt iodization (USI), have significantly reduced prevalence.
Continual monitoring is essential to prevent resurgence in endemic areas.
Iodine deficiency disorders (IDDs) affect millions of children worldwide. Regions with low soil iodine content show higher prevalence rates, emphasizing the need for population-level interventions.
Clinical Features in Children
Clinical manifestations include neck swelling, delayed growth, poor school performance, lethargy, and delayed puberty. Severity depends on the degree and duration of iodine deficiency.
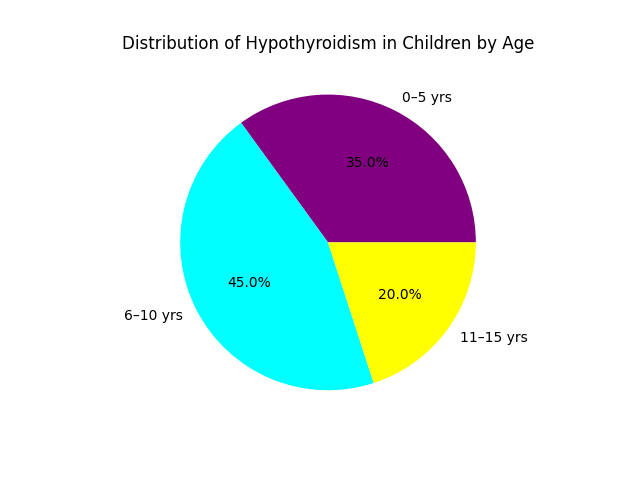
In children, endemic goiter and hypothyroidism represent a spectrum of disorders known as Iodine Deficiency Disorders (IDD). The clinical features vary significantly depending on the age of onset (fetal, neonatal, or juvenile) and the severity of iodine deficiency.
1. Primary Clinical Features
The clinical presentation in children is dominated by three main categories: physical growth retardation, neurodevelopmental delays, and localized thyroid enlargement.
Goiter (Thyroid Enlargement): This is the most visible sign. It is a compensatory mechanism where the thyroid gland enlarges to capture more iodine. In endemic areas, the Total Goiter Rate (TGR) is used as a public health marker.
Growth Retardation (Short Stature): Thyroid hormones (T_3 and T_4) are essential for the production and action of Growth Hormone (GH). Children with chronic hypothyroidism exhibit "catch-down" growth, falling behind their peers on height charts.
Delayed Skeletal Maturation: There is a marked delay in "bone age" compared to chronological age. This is often assessed via X-rays of the hand and wrist, showing delayed appearance of ossification centers.
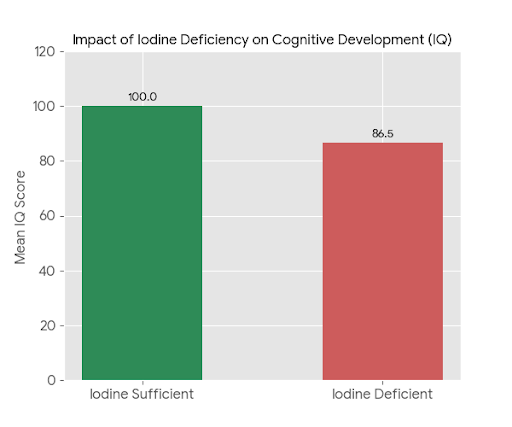
Cognitive and Intellectual Impairment: Even mild iodine deficiency can lead to a shift in the population's intelligence distribution, reducing average IQ scores and increasing the need for special education.
2. Frequency of Symptoms in Children
The chart below illustrates the approximate prevalence of common clinical signs in children suffering from hypothyroidism and iodine deficiency. Growth retardation and delayed bone age are the most consistent clinical markers.
Lethargy and Fatigue: Metabolism slows down, leading to decreased physical activity and "brain fog."
Cold Intolerance: Due to a reduced basal metabolic rate (BMR), children feel cold even in warm environments.
Physical Appearance: Features include a puffy face (myxedema), a large protruding tongue (macroglossia), and dry, coarse skin.
3. Neurodevelopmental Impact: The IQ Shift
One of the most critical public health perspectives of endemic iodine deficiency is its effect on the "brain potential" of a community.
Studies have shown that children in iodine-deficient areas lose an average of 10 to 15 IQ points compared to children in iodine-sufficient areas.
This shift (illustrated above) means that a much larger proportion of the population falls into the "intellectual disability" range, while the number of "gifted" individuals is significantly reduced. This has profound long-term economic and social implications for affected regions.
4. Public Health Perspective: Goiter Prevalence
The severity of iodine deficiency in a population is classified by the WHO based on the prevalence of goiter among school-age children (6–12 years).
Mild Deficiency: TGR between 5% and 19.9%.
Moderate Deficiency: TGR between 20% and 29.9%.
Severe Deficiency: TGR 30%. At this level, cases of Endemic Cretinism (the most severe form of IDD) typically appear.
5. Severe Spectrum: Endemic Cretinism
In regions with extreme iodine deficiency, two types of cretinism are observed:
Neurological Cretinism: Characterized by severe intellectual disability, deaf-mutism, and spasticity (stiff limbs). It results from iodine deficiency during the first and second trimesters of pregnancy.
Myxedematous Cretinism: Characterized by severe growth failure (dwarfism), thickened skin, and signs of severe hypothyroidism. This often results from iodine deficiency continuing into late pregnancy and the neonatal period.
Prevention and Control
Universal salt iodization (USI) is the most effective preventive strategy. Regular monitoring of iodine content in salt and public awareness programs are essential.
1. Public Health Strategies for Prevention
Public health efforts focus on Primordial and Primary Prevention to ensure the environment provides sufficient iodine.
Universal Salt Iodization (USI): This is the most cost-effective and sustainable strategy recommended by the WHO and UNICEF. It involves adding iodine (usually as potassium iodate) to all salt intended for human and animal consumption.
Goal: At least 90% of households should use adequately iodized salt (\geq 15 ppm).
Iodine Supplementation (Iodized Oil): In regions where salt iodization is not yet feasible or where deficiency is severe, oral or injectable iodized oil is administered. This is particularly critical for:
Pregnant Women: To prevent fetal brain damage and congenital hypothyroidism.
Infants and Children: To support cognitive and physical development.
Food Fortification: Beyond salt, other vehicles like bread, milk, and water have been used in specific regions to deliver iodine to the population.
Legislation and Monitoring: Governments must mandate salt iodization through law and establish surveillance systems to monitor salt iodine levels at the production, retail, and household levels.
2. Clinical Perspective and Management
From a clinical standpoint, prevention involves screening and early treatment to avoid the permanent sequelae of hypothyroidism.
Newborn Screening: Universal screening for congenital hypothyroidism (via TSH levels from a heel prick) allows for immediate treatment with Levothyroxine, preventing irreversible mental retardation (cretinism).
Monitoring Urinary Iodine Concentration (UIC): Clinicians and public health officials use the median UIC in school-age children as a "biomarker" to assess the iodine status of the community.
Management of Goiter: In children, most endemic goiters are "nontoxic" and can regress with the introduction of adequate dietary iodine. However, if the goiter is large or causes obstructive symptoms, medical or surgical intervention may be required.
Conclusion
Endemic goiter and hypothyroidism in children are preventable conditions. Early detection and sustained public health measures can significantly reduce disease burden and improve child health outcomes.
The conclusion of a public health and clinical study on Endemic Goiter and Hypothyroidism in Children typically focuses on the critical link between iodine nutrition, thyroid health, and cognitive development.
Below is an explanation of the core conclusions supported by representative data and visualizations.
1. Public Health Success: The Power of Intervention
The primary conclusion of most public health perspectives is that Endemic Goiter is highly preventable. Through Universal Salt Iodization (USI) and clinical monitoring, regions that previously suffered from goiter rates exceeding 30% (severe deficiency) can see these rates drop below the 5% public health threshold within a decade.
Observation: Consistent public health policy (like mandatory salt iodization) leads to a rapid decline in visible goiter and subclinical hypothyroidism.
2. Clinical Impact: Cognitive and Developmental Protection
A critical clinical conclusion is that iodine deficiency is the leading preventable cause of brain damage worldwide. Children in iodine-deficient areas typically exhibit lower cognitive performance compared to those in iodine-sufficient areas.
Key Metric: Studies often report an average IQ deficit of approximately 13.5 points in children from severely iodine-deficient communities.
Clinical Significance: Ensuring adequate iodine intake during pregnancy and early childhood is vital to preventing irreversible neurological damage and "cretinism" (severe congenital hypothyroidism).
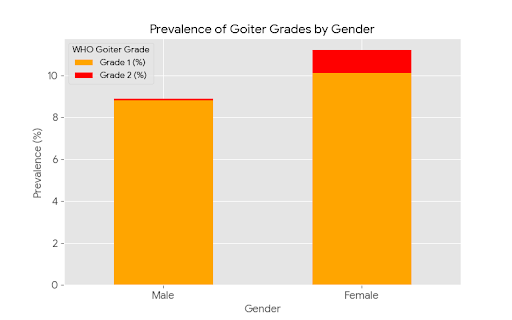
3. Demographic Vulnerability: Gender and Severity
Clinically, the prevalence of goiter is often higher in females and adolescents due to increased physiological demand for thyroid hormones during puberty.
WHO Grading: Public health surveys use the WHO Grading system (Grade 0: None, Grade 1: Palpable, Grade 2: Visible). Most endemic cases are Grade 1 (palpable), but without intervention, Grade 2 (visible) cases increase, leading to secondary complications like respiratory obstruction or swallowing difficulties.
Data and Visualizations
The following charts illustrate these conclusions based on global public health benchmarks and representative clinical data:
Intervention Impact: Shows how goiter prevalence significantly decreases following the implementation of iodine fortification programs.
Cognitive Impact (IQ): Highlights the disparity in average IQ scores between iodine-sufficient and iodine-deficient child populations.
Gender Distribution: Displays the higher prevalence of goiter in females and the distribution of severity (Grade 1 vs. Grade 2).
References.
1.Stanbury JB, Brownell GL, Riggs DS, Perinetti H, Itoiz J, Del Castillo EB. Endemic Goiter: The Adaptation of Man to Iodine Deficiency. Harvard University Press; 1954
2.Eastman C, Zimmermann MB. The Iodine Deficiency Disorders. In: Endotext. Feingold KR, et al., Editors. MDText.com, Inc.; 2000–2018.
3.Lopez SG., Hetzel BS. Endemic goitre and iodine deficiency disorders—etiology, epidemiology and treatment. PubMed. 1988;
4.Clinical practice guidelines “Management of iodine deficiency disorders.” PubMed. — includes protocols for assessment and treatment of endemic goiter and related disorders in children and adults.
5.Prevalence of Iodine Deficiency among School Children … Kyrgyzstan. MDPI Children. 2021 study on goiter prevalence in school-age children.
6.Iodine status reports (World Health Organization, UNICEF, ICCIDD) — global data on iodine deficiency and public health impact.
7.Дедов И.И., Мельниченко Т.А., Фадеев В.Ф. Эндокринология. М.: ГЭОТАР‑Медиа; 2007. – leading Russian endocrinology textbook frequently cited in thyroid disease research.
8.Малая энциклопедия врача‑эндокринолога / Под ред. А.С. Ефимова. Медкнига; 2007 — clinical definition and prevention of endemic goiter
9.Кравцова О.Н., Сагитова Е.Р., Аверьянов В.Н. The problem of iodine deficiency in children (in Vrach). — Russian clinical observation on pediatric IDD.
10.Забаровская З.В., Курмачева Н.А., и др. Заболевания щитовидной железы, обусловленные дефицитом йода.
11.World Health Organization & UNICEF. Iodine Deficiency Disorders global reports — major public health policy and monitoring documents used worldwide.