Contraception
1. Aidarbek K.A
2. Sharmila Marimuthu
3. Chellammal Manikandan
(1, Professor, Department of General Medicine, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.
2,3. Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.)
ABSTRACT
Contraception encompasses a broad array of medical and behavioural methods designed to prevent unintended pregnancy and allow individuals and couples to plan if and when they wish to conceive, with significant implications for reproductive health, quality of life, and public health outcomes; modern family planning strategies combine hormonal, barrier, intrauterine, surgical, and natural approaches, each with distinct mechanisms of action, effectiveness profiles, indications, contraindications, and evolving innovations that respond to both clinical and sociocultural needs in obstetrics and gynaecology, emphasizing patient-centred education and evidence-based choice
Keywords: contraception, birth control, family planning, hormonal methods, intrauterine devices, long-acting reversible contraception, contraindications, recent advances.
INTRODUCTION
Contraception is defined as the intentional prevention of conception through the use of various chemical, physical, behavioural, or surgical methods that interfere with the normal process of fertilization or implantation. Its role in obstetrics and gynaecology extends beyond simply preventing pregnancy to include regulation of menstrual cycles, reduction of dysmenorrhea, lowering the risk of certain gynaecologic cancers, and supporting broader reproductive health goals. The global adoption of contraceptive methods has grown substantially, with practitioners and patients navigating an expanding array of options grounded in both historical practice and modern scientific innovation.
Objectives: The primary objective of contraception is to enable individuals to avoid or delay pregnancy in accordance with personal, health, and family planning goals. Secondary objectives include reduction of unintended pregnancies and associated complications, management of menstrual disorders, and broader social and health benefits, such as improved maternal health outcomes.
CLASSIFICATION OF CONTRACEPTION AND MECHANISM OF ACTION
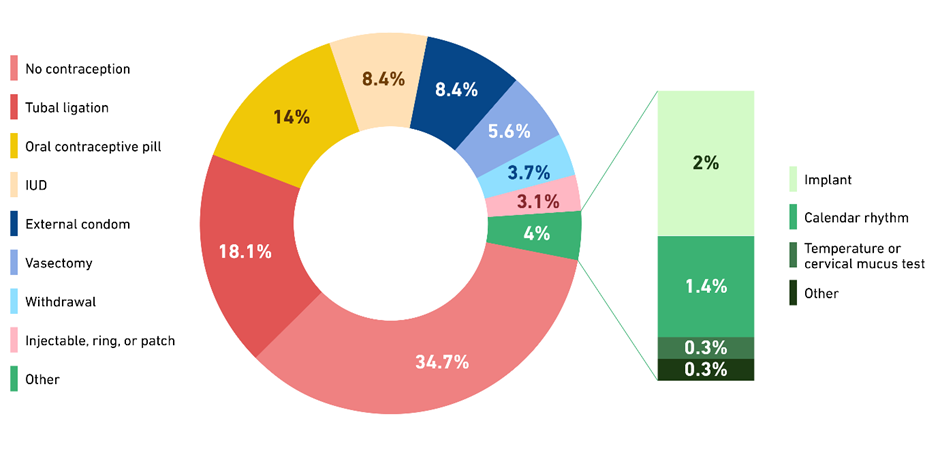
Contraceptive methods are broadly classified into natural, barrier, hormonal, intrauterine, long-acting reversible contraception (LARC), surgical, and emergency methods. Natural methods like fertility awareness rely on tracking physiological signs to avoid intercourse during fertile windows. Barrier methods physically block sperm, as with condoms and diaphragms. Hormonal methods, including combined oestrogen-progestin and progestin-only pills, patches, injections, and implants, prevent ovulation, thicken cervical mucus to inhibit sperm penetration, and alter the endometrium to reduce implantation likelihood. LARCs such as intrauterine devices (IUDs) and implants provide extended contraception with minimal user action; copper IUDs create a spermicidal intrauterine environment through localized inflammatory changes, while hormonal IUDs continuously release progestins to suppress ovulation and alter cervical mucus. Surgical methods, including tubal ligation and vasectomy, permanently occlude reproductive pathways.
DETAILED DESCRIPTION OF MAJOR CONTRACEPTIVE METHODS
Hormonal contraceptives include combined oral contraceptives, which use synthetic oestrogen and progestin to suppress the hypothalamic-pituitary-ovarian axis, and progestin-only methods such as implants like the levonorgestrel-releasing subdermal device, which provides highly effective long-term contraception with a failure rate often below 1% per year. Barrier methods like condoms provide protection against sexually transmitted infections, in addition to preventing pregnancy. Intrauterine devices, available in copper and hormonal forms, are among the most effective reversible options, lasting from 3 up to 12 years depending on the device, and are widely used globally.
INDICATIONS FOR CONTRACEPTIVE USE
Contraception is indicated for sexually active individuals wishing to prevent pregnancy, those with medical conditions that make pregnancy high risk, and individuals seeking to manage menstrual disorders or non-contraceptive health benefits of hormonal methods. Contraceptive choice should be individualized based on age, lifestyle, reproductive goals, and medical history to optimize both effectiveness and safety.
CONTRAINDICATIONS
Contraindications to specific contraceptives are informed by evidence-based criteria such as the World Health Organization Medical Eligibility Criteria, which categorize conditions where use is safe, requires caution, or is contraindicated outright; for instance, combined hormonal contraceptives may be contraindicated in individuals with certain cardiovascular risk factors, active liver disease, or hormone-sensitive cancers, while progestin-only methods may be preferred where oestrogen exposure poses risk.
RECENT ADVANCES IN CONTRACEPTION
Recent advances in contraception include development of new hormonal formulations with improved side-effect profiles, over-the-counter progestin-only pills to expand access, and innovative delivery systems such as contraceptive microchips and microneedle patches currently under research. Emerging non-hormonal methods, including agents that modulate the vaginal environment to prevent sperm mobility, are also being investigated to broaden choices. These innovations aim to improve effectiveness, acceptability, and accessibility, with ongoing research shaping future options in reproductive health.
CONCLUSION
Contraception remains a fundamental component of obstetrics and gynaecology, integrating a range of methods that empower individuals to make informed reproductive choices. With continuous advances in technology and a deepening understanding of patient needs, clinicians must remain well-versed in contraceptive mechanisms, benefits, risks, and evolving evidence to support personalized care and advance public health outcomes.
REFERENCES
Female and Male Contraception* (Springer, 2021)
*The Handbook of Contraception: A Guide for Practical Management* (Springer, 2016)
*Contraception* (Elsevier)
*The European Journal of Contraception & Reproductive Health Care*
[1]: https://pubmed.ncbi.nlm.nih.gov/25905371/?utm_source=chatgpt.com "Contraception - PubMed"
[2]: https://www.ncbi.nlm.nih.gov/books/NBK279148/?utm_source=chatgpt.com "Contraception – Endo text - NCBI Bookshelf"
[3]: https://en.wikipedia.org/wiki/Copper_IUD?utm_source=chatgpt.com "Copper IUD"
[4]: https://pharmaceutical-journal.com/article/ld/hormonal-contraception-methods-and-patient-eligibility?utm_source=chatgpt.com "Hormonal contraception: methods and patient eligibility - The Pharmaceutical Journal"
[5]: https://academic.oup.com/biolreprod/article/110/1/14/7370244?utm_source=chatgpt.com "Reversible female contraceptives: historical, current, and future perspectives‡ | Biology of Reproduction | Oxford Academic"
[6]: https://link.springer.com/book/10.1007/978-3-030-70932-7?utm_source=chatgpt.com "Female and Male Contraception | Springer Nature Link (formerly SpringerLink)"