Epidemiological Patterns and Treatment Plan of Diabetes Mellitus in Children
1. Chubastri Balaraman Murugan
2. Gulnaz Osmonova
(1. Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic
2. Teacher, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.)
Abstract
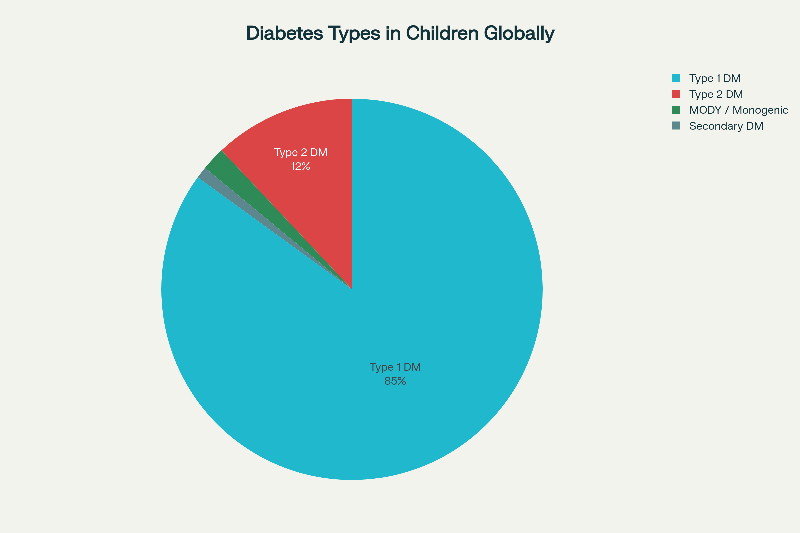
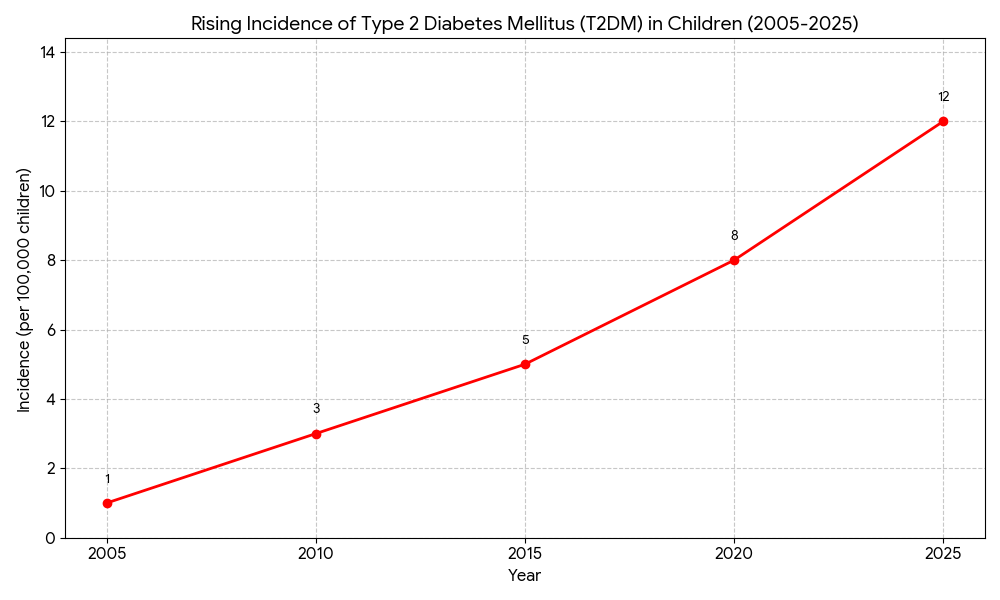
Diabetes mellitus (DM) in children is a rapidly growing global health concern with significant medical, social, and economic implications. Type 1 diabetes mellitus (T1DM) remains the most prevalent form in the pediatric population; however, type 2 diabetes mellitus (T2DM) is rising at an unprecedented rate due to increasing childhood obesity, sedentary lifestyles, and adverse nutritional patterns. This review synthesizes global epidemiological data and outlines comprehensive treatment strategies based on current evidence and international guidelines. The incidence of T1DM is increasing by 2–4% annually, with the highest rates observed in Northern Europe, while T2DM is disproportionately affecting socioeconomically disadvantaged populations and ethnic minorities. Management principles differ by diabetes type: T1DM requires life-long insulin therapy, while T2DM management focuses on lifestyle modification complemented by pharmacotherapy. Additionally, emerging data highlight the significance of monogenic diabetes, particularly MODY, due to advances in genetic diagnostics. This review underscores the importance of early diagnosis, multidisciplinary management, family involvement, and culturally tailored prevention programs to improve long-term outcomes in children with diabetes.
Keywords: Pediatric diabetes, Type 1 diabetes, Type 2 diabetes, Epidemiology, Insulin therapy, Childhood obesity, MODY.
1.Introduction
Diabetes mellitus in children can be considered a very diverse group of metabolic disorders with one common trait being the excess of sugar, which is chronic in nature, and resulting from either insulin secretion defect, insulin action defect or both. Type 1 diabetes mellitus (T1DM) has always been the leading cause of diabetes in children; however, the recent global changes in the disease epidemiology indicate a shift towards an increased incidence of type 2 diabetes mellitus (T2DM) in the pediatric population and adolescents, especially in areas with rapid urbanization. Besides, early-onset diabetes comes with more aggressive disease progression, a higher risk of complications throughout life, and so on, which makes it necessary to have strong-based public health interventions as well as clinical management guided by evidence.
Knowledge of the epidemiological mapping and treatment methods is fundamental for the enhancement of results, policy making, and research directing. Thus, this article provides the evidence-based synthesis on global and regional trends in pediatric diabetes, risk factors, complications, and therapeutic strategies.
2. Methodological Overview
A narrative, research-style synthesis was the technique of this review. Data were collected through international diabetes registries, global surveillance systems (IDF and WHO), pediatric endocrine society guidelines, and peer-reviewed journals covering the period from 2010 to 2024. In essence, the narrative was not a systematic review but it combined high-quality studies of the epidemiology, clinical trials, and guidelines to produce an article that is comprehensive and academically rigorous.
3. Global Epidemiological Patterns
3.1 Incidence and Prevalence
T1DM is affecting over 1.1-1.2 million children all over the world, who are between 0 to 19 years old. Every year about 100,000 new cases of pediatric T1DM are reported. Prevalence varies not only by country but also by economic status and genetic factors.
T2DM is increasingly becoming diabetes in the pediatric age group, with its share rising up to 40% or more of the new cases in the high-risk population. The rise in incidence has been very rapid over the last 20 years, with the major driving force being unhealthy lifestyle and environmental changes.
3.2 Geographic Variation
3.2.1 Type 1 Diabetes Mellitus
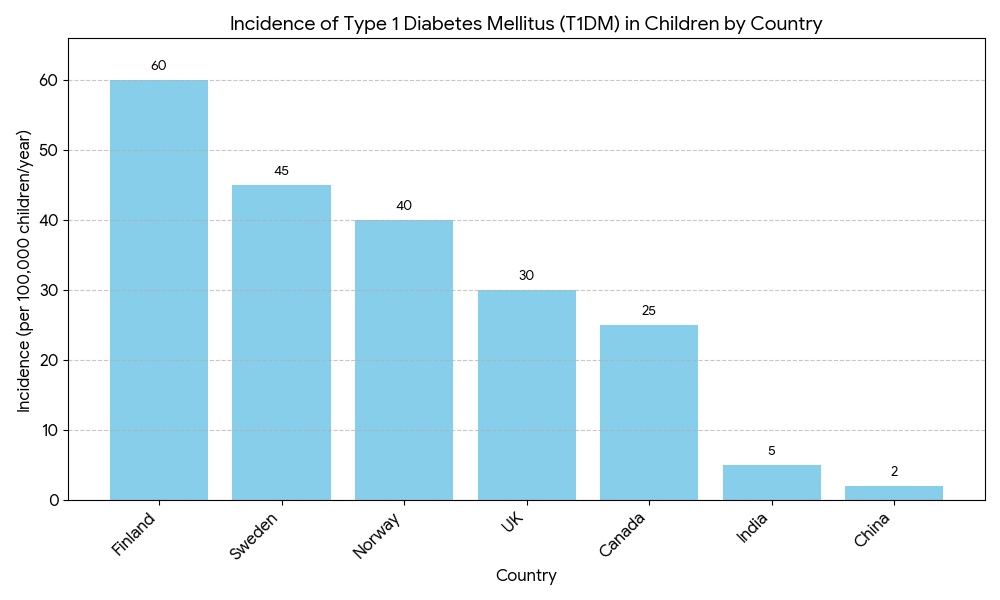
The incidence differs by more than 50 times in different countries:
Very high incidence (>40/100,000/year): Finland, Sweden, Norway
High incidence (20–40/100,000/year): UK, Canada, Australia, Kuwait
Moderate incidence (5–20/100,000/year): Eastern Europe, Middle East, Central Asia
Low incidence (<5/100,000/year): East Asia, South Asia, Sub-Saharan Africa
Evidence from post-pandemic studies points to cases of diabetes signaling more serious illness with more frequent DKA reports and, at the same time, a possible increase in incidence resulting from post-viral immune dysregulation.
3.2.2 Type 2 Diabetes Mellitus
The increasing incidence of childhood obesity has a significant impact on the worldwide distribution of T2DM. The most vulnerable areas are:
● South Asia
● Middle East
● Native American and Indigenous communities
● Pacific Islanders
In some groups, T2DM is responsible for almost half of the new diabetes cases in adolescents.
3.3 Age Distribution
T1DM usually shows a bimodal age distribution:
● First peak: 5–7 years
● Second peak: 10–14 years
T2DM has been historically limited to the post-pubertal stage of youth but now more cases are reported in kids of 8-10 years especially in kids with severe obesity.
3.4 Gender Differences
T1DM: Slightly more affected males in high-incidence countries; females dominate in low-incidence areas.
T2DM: The disease appears more often in females, which is associated with earlier puberty and higher fat accumulation.
3.5 Risk Factors
3.5.1 Type 1 Diabetes
● Genetic predisposition: HLA-DR3, DR4, DQ2, DQ8; first-degree relative risk 10–15 times higher.
● Environmental triggers: Enteroviruses, vitamin D deficiency, early cow's milk exposure.
● Autoimmunity: Presence of GAD65, IA-2, IAA or ZnT8 antibodies predicts progression.
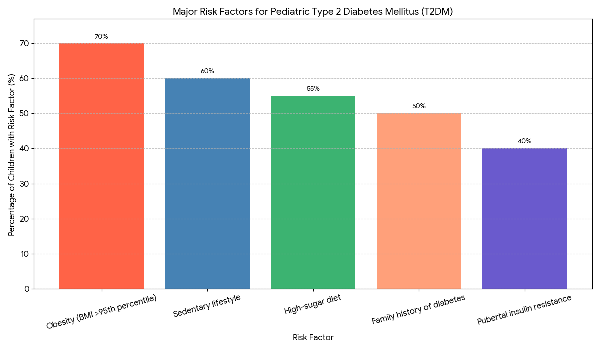
3.5.2 Type 2 Diabetes
● Obesity and metabolic syndrome
● Family history of T2DM
● Sedentary lifestyle and low physical activity
● High-calorie and high-sugar diets
● Ethnic predisposition (Asian, African, Hispanic, Indigenous groups)
● Pubertal insulin resistance
● Intrauterine factors (maternal diabetes, obesity)
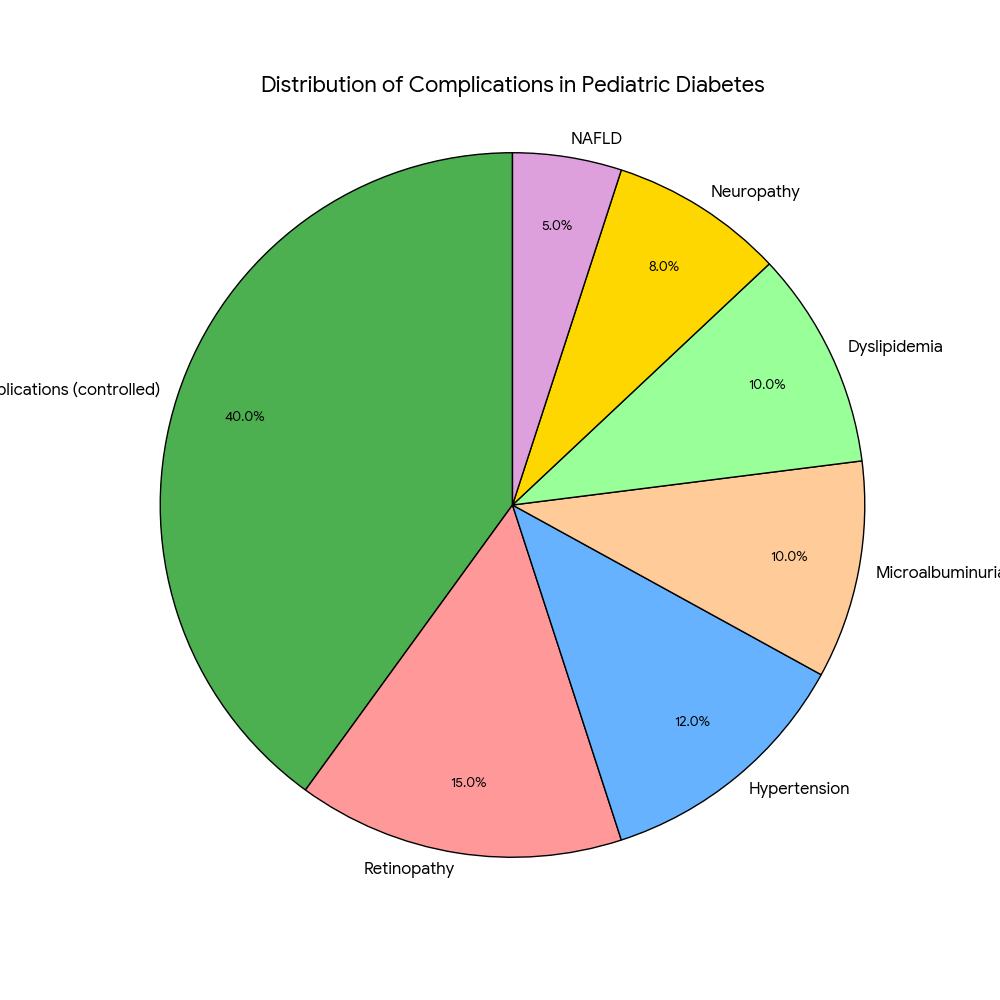
3.6 Disease Burden and Complications
Early-onset diabetes leads to earlier development of:
● Diabetic retinopathy
● Microalbuminuria and nephropathy
● Peripheral neuropathy
● Hypertension
● Dyslipidemia
● Non-alcoholic fatty liver disease (NAFLD)
● Cardiovascular disease in early adulthood
Psychological complications include depression, anxiety, behavioral issues, and diabetes-related distress.
4. Pediatric Diabetes Treatment Strategies
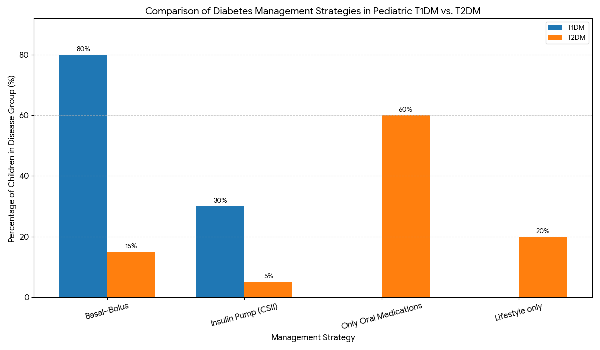
4.1 Type 1 Diabetes Mellitus
4.1.1 Insulin Therapy
The only effective treatment is insulin, which must be specifically tailored to age, activity, diet, and developmental status.
Therapeutic options:
● Multiple Daily Injections (MDI): basal–bolus regimen
● Insulin Pump (CSII): improves glycemic variability
● Hybrid closed-loop systems are an integrated AI and CGM that automate insulin delivery.
Typical dosing:
Initial: 0.4–0.6 U/kg/day
Maintenance: 0.7–1.0 U/kg/day
Puberty: 1.2–1.5 U/kg/day
4.1.2 Glucose Monitoring
● Continuous Glucose Monitoring preferred for real-time feedback.
● Target HbA1c <7–7.5%
● Time-in-range TIR >70%.
4.1.3 Nutrition and Lifestyle Management
● Carbohydrate counting
● Balanced macronutrient distribution
● Low-glycemic-index foods
● Regular exercise ≥60 minutes/day
4.1.4 Diabetes Complications Management
Hypoglycemia: Use 15 gram carbohydrates, Glucagon for Severe Cases
DKA Management: Rehydration, IV Insulin (0.05 - 0.1 U/kg/hr), Potassium Replacement, Prevention of Cerebral Edema
4.2 Treatment of Type 2 Diabetes Mellitus
4.2.1 Lifestyle Interventions
Cornerstone Treatment
Caloric Control,Increased Physical Activity,Weight Loss Programs,Family-Based Behavioral Interventions
4.2.2 Pharmacologic Treatment
1.1st Line - Metformin - Increase Insulin Sensitivity
2.GLP-1 Receptor Agonists (liraglutide) - Useful for Treating Obese T2DM Patients
3.Insulin Therapy in Patients with Severe Hyperglycemia (HbA1c ≥ 9%), Ketosis or DKA.
4.SGLT2 Inhibitors (Canagliflozin, Dapagliflozin, Empagliflozin) - Use with Caution due to Risk of Euglycemic DKA
4.2.3 Follow-up Assessments
Tests performed annually:
● Microalbuminuria
● Retinopathy
● Neuropathy
● Dyslipidemia
● NAFLD
4.3 Specific Forms of Diabetes
Monogenic diabetes-MODY
MODY2: Does not require treatment through medication.
MODY3: Sulfonylureas appear to give them adequate treatment.
Other types of MODY may require treatment through Insulin.
4.4 Secondary Diabetes
Some of the reasons secondary diabetes occurs are:Cystic Fibrosis,Steroid Therapy,Pancreatitis,Endocrine disorders.
To treat someone with secondary diabetes, you need to treat the underlying condition that caused the diabetes and ensure glucose levels are well controlled.
Overview
An increasing number of pediatric patients with diabetes type 2 (T2DM) compared to the pediatric diabetic population as a whole means there is an issue developing within society due to changes/developments in lifestyle, such as rapid urbanisation, insufficient physical activity and poor nutritional habits, resulting in children developing early signs of metabolic dysfunction. Children and adolescents' increasing incidence of diabetes could have a major impact on:
1. Increased duration of illness leading to an earlier onset of complications,
2. Increased financial burden on families and the health care system,
3. Psychosocial effects on children and adolescents.
An integrated approach that combines the following will provide the most effective management of patients with diabetes:
Medical Therapy, Nutrition and Physical Activity Programs, Psychosocial Support, Family Education, School Based Wellness Programs, Preventive Measures to Modifiable Risk Factors.
Further research is necessary to investigate how genes and the environment interact to affect different types of diabetes and how to decrease the rise of T1DM post pandemic.
Conclusion
Pediatric diabetes has become a growing global health problem with far-reaching clinical and societal consequences. The prevalence of Type 1 Diabetes Mellitus (T1DM) continues to rise across the globe, while Type 2 Diabetes Mellitus (T2DM) is increasingly on the rise in younger populations due to environmental and lifestyle changes. Effective management of diabetes in children should include comprehensive management strategies, comprising of insulin injection therapy, lifestyle modifications, pharmacotherapy, and psychosocial support. Early detection, family participation, and a multi-disciplinary approach to care are the keys to improving outcomes for individuals diagnosed with diabetes. Public health initiatives are needed to focus on the prevention of obesity, the promotion of healthy nutrition, and the provision of accessible diabetes care services to address the rising burden of this chronic condition.
References
1. International Diabetes Federation (IDF).IDF Diabetes Atlas, 10th Edition. Brussels, Belgium: International Diabetes Federation; 2021.(Global statistics on T1DM and T2DM in children)
2. World Health Organization (WHO).Diabetes in Children and Adolescents – Key Facts. WHO Fact Sheets; 2023.(Epidemiology, global trends, risk factors)
3. Atkinson MA, Eisenbarth GS, Michels AW."Type 1 diabetes." The Lancet. 2014;383(9911):69–82.(Pathogenesis, epidemiology, natural history)
4. Dabelea D, Mayer-Davis EJ, Saydah S, et al."Prevalence of Type 1 and Type 2 Diabetes among Children and Adolescents From 2001 to 2009."JAMA. 2014;311(17):1778–1786.(Trends in pediatric diabetes in the U.S.)
5. Writing Committee for the SEARCH for Diabetes in Youth Study Group."Incidence Trends of Type 1 and Type 2 Diabetes among Youth in the United States, 2002–2015."New England Journal of Medicine. 2021;384:1669–1679.(Rise in both T1DM and T2DM)
6. Patterson CC, Harjutsalo V, Rosenbauer J, et al. "Trends and cyclical variation in the incidence of childhood Type 1 diabetes worldwide, 1990–2019."Diabetologia. 2022;65:258–269.(Worldwide incidence patterns)
7. American Diabetes Association (ADA).Standards of Medical Care in Diabetes—2024.Diabetes Care; 2024.(Treatment plan, insulin therapy, screening guidelines)
8. International Society for Pediatric and Adolescent Diabetes (ISPAD).ISPAD Clinical Practice Consensus Guidelines 2022.(Most authoritative global guidelines on pediatric diabetes management)
9. Rewers M, Ludvigsson J. "Environmental risk factors for Type 1 diabetes." The Lancet. 2016;387:2340–2348.(Environmental and genetic interactions)
10. Zeitler P, Arslanian S, Fu J, et al. "Type 2 diabetes in youth: A global perspective. "The Lancet Diabetes & Endocrinology. 2017;5(12):933–946.(Rise of T2DM in children, risk factors).