Diabetes Insipidus in Children
1. Osmonova G. Zh
2. Ishant Nimbalkar
(1. Teacher, Dept. of Pediatrics, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic
2.Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
ABSTRACT
Diabetes insipidus (DI) is a rare disorder of water regulation that is particularly characterized by the excretion of large quantities of dilute urine and thirst due to a deficiency of antidiuretic hormone (ADH) or an impairment of its responsiveness. Pediatric diabetes insipidus is particularly challenging to diagnosis because the presentation of the disorder may overlap with that of other more common childhood conditions such as diabetes mellitus, urological disorders, or psychiatric polydipsia. The disorder can either be congenital or acquired. Indeed, it has been classified into three types: central diabetes insipidus, nephrogenic diabetes insipidus, and primary polydipsia. Pediatric diabetes insipidus, which has a small disease burden, can progress to cause severe complications such as dehydration, hypernatremia, growth retardation, and central nervous system damage should it remain untreated. Early diagnosis and treatment of the condition, however, can have a great impact. The review seeks to discuss the etiology, pathophysiology, diagnosis, differential diagnosis, management, and follow-up of diabetes insipidus in children.
INTRODUCTION
A relatively rare but serious general Accepted condition is diabetes insipidus, which is related to the body’s failure to manage its water balance properly. The causes may be the inadequate secretion of antidiuretic hormone, also known as the Arginine-vasopressin hormone, by the posterior lobe of the pituitary gland, as well as its resistance in the kidneys. The condition is more serious in pediatrics, as small children and babies are poor in expressing their need to have a certain amount of fluid to avoid the complication related to dehydration.
The condition is characterized by polyuria, polydipsia, associated with the inability to concentrate urine, resulting in frequent urination of a large amount of diluted urine. Diabetes insipidus can occur at any age from infancy to adolescence because it can be acquired or congenital due to trauma, malignancy, infection, or autoimmune diseases of the hypothalamic-pituitary system. The nephrogenic type of diabetes insipidus can be either inherited or secondary to metabolic diseases.
In spite of its relative rarity among pediatric endocrine conditions, diabetes insipidus may result in growth retardation, recurrent dehydration, hypernatremia, seizures, and impaired neurodevelopment if there is significant delay in diagnosis. Diagnosis accuracy improved with improvements in diagnostic techniques such as water deprivation testing, desmopressin response testing, and neuroimaging. The long-term prognosis has greatly improved with effective treatment strategies, especially the use of desmopressin for central diabetes insipidus.
The General Epidemiology of Diabetes Insipid
Globally, the number of cases affected by DI is low; its prevalence rate is estimated at 1:25,000 in the general population.
The Incidence rate (new cases) of DI has been estimated around 3 per 100,000 per year.
Children Specifically
DI may happen in any age group, including in pediatric cases, though this is largely not accounted for in big studies, as incidence is very rare.
Incidence of congenital nephrogenic DI, which is the inherited form, in males occurs at a rate of between 4 and 8 in every 1 million births due to the X-linked form.
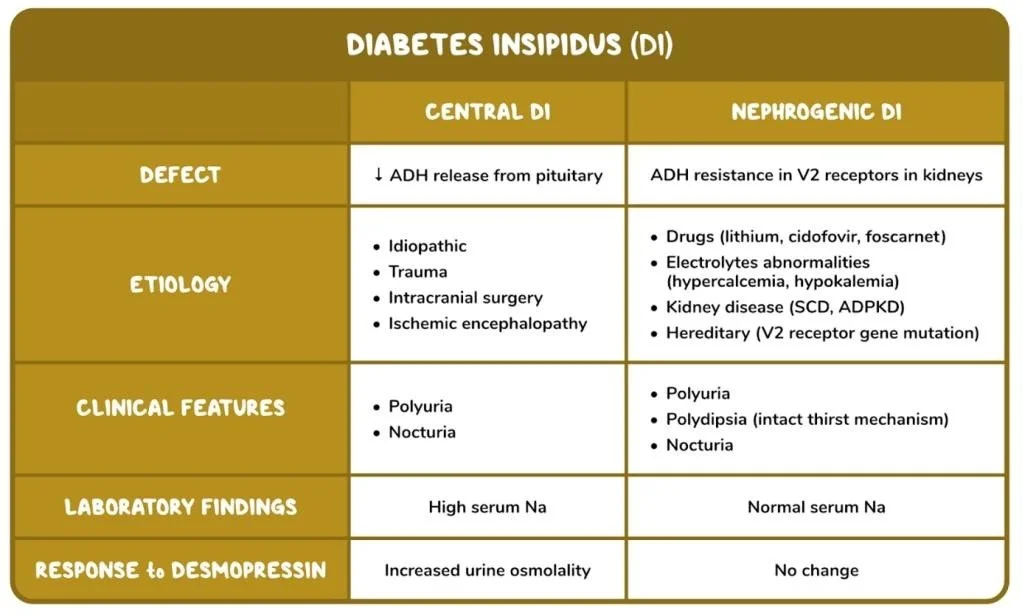
Types of Diabetes Insipidus
1. Central (Neurogenic) DI
→ Deficient ADH secretion
Pathogenesis:
↓ ADH → ↓ water reabsorption → large volumes of dilute urine → dehydration → hypernatremia
2. Nephrogenic DI
→ Kidneys unresponsive to ADH
Pathogensis:
Normal or high ADH → kidney cannot respond → persistent polyuria
Clinical features
Infants
Poor feeding, Failure to thrive, Irritability, Fever without infection, Vomiting, Dehydration, Wet diapers very frequently
Older Children
Polyuria (large volumes, dilute urine)
Polydipsia (strong preference for cold water)
Nocturia / enuresis
Fatigue
Headache
Growth retardation (chronic cases)
Severe / Untreated
Dehydration
Hypernatremia
Seizures
Altered consciousness
Methods
Etiology, Pathophysiology, and Diagnostic Etiology Central Diabetes Insipidus
Genetic: Mutations of the AVP gene Idiopathic (20–50%)
Tumors: Craniopharyngioma, germinoma, LCH Trauma: Head injury, neurosurgical complications
Infections: TB, meningitis, encephalitis
Autoimmune hypophysitis
Ischemic/hypoxic injury: Perinatal asphyxis Nephrogenic Diabetes Insipidus
Congenital:
AVPR2 mutation (X-linked) AQP2
Mutation (autosomal)
Acquired:
Drugs: Lithium, amphotericin B, demeclocycline Electrolyte disturbances: Hypercalcemia, hypokalemia, CKD
Obstructive uropathy
Treatment
Central DI
Desmopressin (DDAVP) – drug of choice
Oral / intranasal / parenteral
Dose individualized
Avoid overcorrection
Complication: water intoxication → hyponatremia
Conclusion
Diabetes Insipidus in children is an uncommon occurrence worldwide as well as in the Indian population. There isn’t an exact figure from the Indian population regarding affected children due to its rarity and lack of population registries for such conditions. The approximate prevalence from worldwide estimates is 1:25,000 population for DI, and congenital nephrogenic DI is an even rarer occurrence.
In the majority of cases that have been reported from India, it appears that it is relatively rare and that it poses certain clinical challenges because it could lead to severe dehydration and/or neurological damage if it is not diagnosed on time.
References
1.https://journals.lww.com/ipcr/fulltext/2022/02030/transient_diabetes_insipidus_in_a_preterm_neonate_.10.aspx
2.https://pubmed.ncbi.nlm.nih.gov/27540876/?utm_source=chatgpt.com
3. Bichet DG. “Genetic and clinical spectrum of nephrogenic diabetes insipidus.” Nat Rev Nephrol,
4.Robertson GL. “Diabetes Insipidus.” Endocrinol Metab Clin North Am.
5.Arima H, Oiso Y. “Mechanisms of water balance disorders.” Nat Rev Nephrol.
6.Maghnie M et al. “Central diabetes insipidus in children and young adults.” N Engl J Med.