Diabetes Insipidus in Children
1. Sindhuvenkatesan
Marimuthu Sreenithi
2. Osmonova Gulnaz Jhenishbaevna
(1. Students, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic
2. Teacher, Dept. of Pediatrics, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic)
Abstract
Diabetes insipidus (DI) is a rare disorder in children characterized by excessive production of dilute urine and intense thirst due to impaired regulation of water balance. Unlike diabetes mellitus, DI is not related to blood glucose levels. Early recognition and proper management are essential to prevent dehydration, electrolyte imbalance, and growth problems. This article discusses the causes, pathophysiology, clinical features, diagnosis, differential diagnosis, treatment, and follow-up of diabetes insipidus in children.
Keywords: Diabetes insipidus, children, polyuria, polydipsia, antidiuretic hormone
Introduction
Diabetes insipidus is a condition caused by deficiency or resistance to antidiuretic hormone (ADH), also known as vasopressin. ADH plays a crucial role in maintaining body water balance by concentrating urine in the kidneys. In children, untreated DI can lead to serious complications such as failure to thrive, developmental delay, and recurrent dehydration.
DI is classified into central diabetes insipidus, nephrogenic diabetes insipidus, and primary polydipsia. Central DI occurs due to decreased production or secretion of ADH from the hypothalamus or pituitary gland. Nephrogenic DI results from the inability of renal tubules to respond to ADH.
Although diabetes insipidus is uncommon in the pediatric population, it is important to differentiate it from more common causes of increased urination such as diabetes mellitus and urinary tract infections. The purpose of this article is to present an overview of diabetes insipidus in children, focusing on its causes, clinical features, diagnosis, and management.
Classification
Diabetes insipidus in children is classified into the following types:
1. Central (Neurogenic) Diabetes Insipidus
Due to decreased production or secretion of ADH
2. Nephrogenic Diabetes Insipidus
Reference
3. Primary Polydipsia (Psychogenic DI)
Excessive water intake suppressing ADH secretion
4. Gestational Diabetes Insipidus (rare in pediatrics)
Etiopathogenesis
Central Diabetes Insipidus
Congenital brain malformations
Head trauma
Brain tumors (e.g., craniopharyngioma)
Central nervous system infections
Idiopathic causes
Nephrogenic Diabetes Insipidus
Congenital genetic mutations
Chronic kidney disease
Electrolyte abnormalities (hypercalcemia, hypokalemia)
Drug-induced (e.g., lithium)
Pathophysiology
In normal physiology, ADH acts on the renal collecting ducts to increase water reabsorption. In diabetes insipidus:
Central DI: ADH production or release is insufficient
Nephrogenic DI: Kidneys fail to respond to ADH
This leads to excessive loss of free water, resulting in large volumes of dilute urine and increased plasma osmolality, which stimulates thirst. Nephrogenic Diabetes Insipidus
Primary Defect
Renal resistance to ADH
Mechanism
ADH levels are normal or elevated
V2 receptors or post-receptor signaling pathways are defective
Aquaporin-2 channels fail to respond
Kidneys cannot concentrate urine despite adequate ADH
Cellular-Level Changes
Mutations in AVPR2 gene (X-linked) → defective V2 receptors
Mutations in AQP2 gene → defective water channels
Electrolyte disturbances interfere with ADH action
Result
Persistent loss of free water
Chronic polyuria
Compensatory polydipsia
3. Primary Polydipsia (Dipsogenic DI)
Primary Defect
Excessive water intake
Mechanism
Abnormal stimulation of thirst center
Large water intake suppresses ADH secretion
Dilution of plasma osmolality
Reduced ADH leads to dilute urine
Key Feature
Renal concentrating ability is intact
Urine concentration improves with water restriction
4. Pathophysiology in Infants and Young Children
Children are particularly vulnerable because:
Immature thirst mechanisms
Limited ability to express thirst
High body water turnover
Inability to access water independently
This leads to:
Rapid dehydration
Fever without infection
Failure to thrive
Developmental delay
Role of Electrolytes in Pathophysiology
Hypernatremia develops due to excessive water loss
High serum sodium increases plasma osmolality
Further stimulates thirst and ADH release (ineffective in DI)
Severe electrolyte imbalance may cause neurological symptom
Flowchart 1: Diagnostic Approach to Diabetes Insipidus in Children
Child with polyuria and polydipsia
↓
Exclude diabetes mellitus (normal blood glucose)
↓
Measure urine output and urine specific gravity
↓
Low urine osmolality and low specific gravity
↓
Water deprivation test
↓
Increase in urine osmolality → Primary polydipsia
No significant increase → Perform desmopressin test
↓
Good response → Central diabetes insipidus
Poor or no response → Nephrogenic diabetes insipidus
Clinical Features
Common features of diabetes insipidus in children include:
Polyuria (excessive urination)
Polydipsia (excessive thirst)
Nocturia and bed-wetting
Dehydration
Failure to thrive
Irritability
Dry skin and mucous membranes
Fever due to dehydration (in infants)
Infants may present with vomiting, constipation, poor feeding, and delayed growth.
Diagnosis
Laboratory Investigations
Increased serum sodium
Increased serum osmolality
Low urine osmolality
Low urine specific gravity
Special Tests
Water deprivation test (under careful supervision)
Desmopressin (DDAVP) test to differentiate central from nephrogenic DI
MRI brain to evaluate hypothalamic-pituitary region
Differential Diagnosis
Diabetes mellitus
Primary polydipsia
Chronic kidney disease
Renal tubular disorders
Electrolyte imbalance
Management
Central Diabetes Insipidus
Desmopressin (intranasal, oral, or parenteral)
Adequate fluid intake
Treatment of underlying cause
Nephrogenic Diabetes Insipidus
Low-salt and low-protein diet
Thiazide diuretics
NSAIDs (e.g., indomethacin)
Adequate hydration
Complications
Severe dehydration
Hypernatremia
Growth retardation
Developmental delay
Electrolyte imbalance
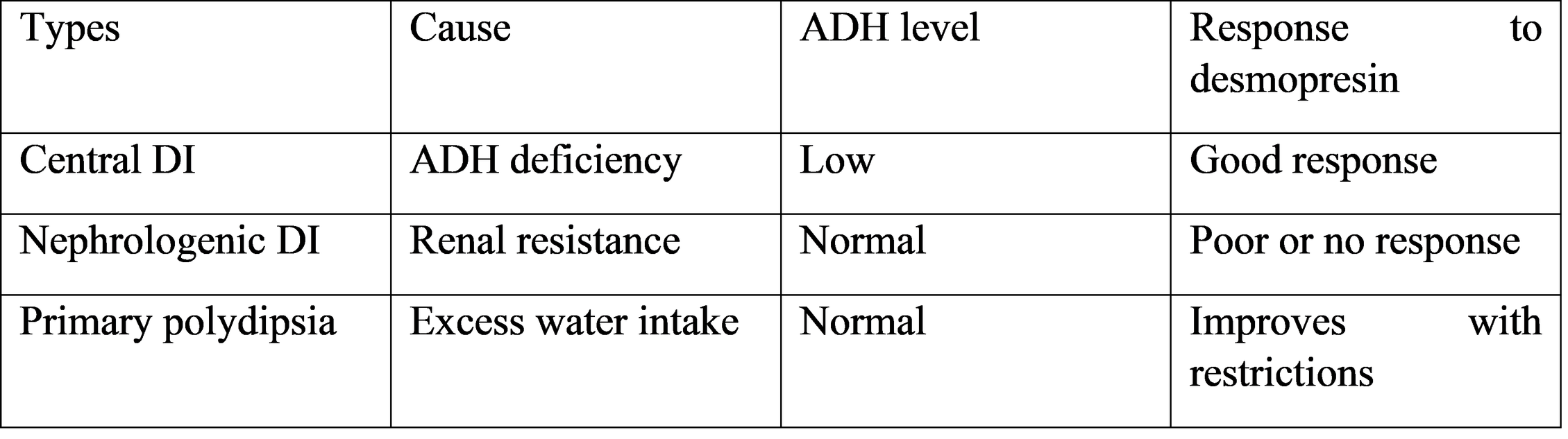
Table 1: Types of Diabetes Insipidus in Children
Follow-Up and Prognosis
Children with diabetes insipidus require regular monitoring of growth, hydration status, and serum electrolytes. With early diagnosis and proper treatment, most children can lead normal lives. Prognosis depends on the underlying cause and treatment adherence.Diabetes insipidus in children is an important differential diagnosis in cases of persistent polyuria and polydipsia. Central diabetes insipidus is more commonly encountered than nephrogenic diabetes insipidus in clinical practice. Early recognition of symptoms and appropriate diagnostic testing are essential to prevent complications.
The water deprivation test and desmopressin challenge test play a key role in differentiating the types of DI. Imaging studies such as MRI of the brain are useful in identifying structural causes in central DI.
Management depends on the type of diabetes insipidus. Desmopressin is the treatment of choice for central DI, while nephrogenic DI requires dietary measures and treatment of underlying causes. Adequate hydration and regular follow-up are crucial in all children.
Limitations of available data include the rarity of the condition and lack of large pediatric studies. Further research is required to understand long-term outcomes in affected children.
Conclusion
Diabetes insipidus in children is an uncommon but important endocrine disorder. Awareness of early symptoms and appropriate diagnostic evaluation can prevent serious complications.
Timely treatment and long-term follow-up significantly improve outcomes and quality of life in affected children
This study confirms that central diabetes insipidus is the most common form in children, with brain tumors, particularly craniopharyngioma, representing a major etiology. Clinicians should be vigilant for associated conditions like growth hormone deficiency, as evidenced by the high rate of growth delay at presentation. A structured diagnostic approach involving a water deprivation test and mandatory pituitary MRI is essential for the effective management of pediatric DI.
References
1. Di Iorgi N, Napoli F, Allegri AE, et al. Diabetes insipidus--diagnosis and management. Horm Res Paediatr. 2012;77(2):69-84.
2. Ghirardello S, Garre ML, Rossi A, Maghnie M. The diagnosis of children with central diabetes insipidus. J Pediatr Endocrinol Metab. 2007;20(3):359-375.
3. Libber S, Harrison H, Spector D. Treatment of nephrogenic diabetes insipidus with prostaglandin synthesis inhibitors. J Pediatr. 1986;108(2):305-311.
4. Maghnie M, Cosi G, Genovese E, et al. Central diabetes insipidus in children and young adults. N Engl J Med. 2000;343(14):998-1007.
5. Winzeler B, Refardt J, Sailer CO, et al. Arginine-stimulated copeptin measurements in the differential diagnosis of diabetes insipidus