Diabetes Mellitus in Children
1. Manickavel Surya Nithish
2. Osmonova G. Zh.
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Teacher, International Medical Faculty, Osh State University, Kyrgyzstan)
Abstract:
Diabetes mellitus in childhood is a significant and growing public health challenge worldwide. This article explores the epidemiology, pathophysiology, clinical features, diagnosis, management, complications, and preventive strategies relevant to children and adolescents. We include key graphs and diagrams to illustrate important trends and mechanisms.
1. Introduction
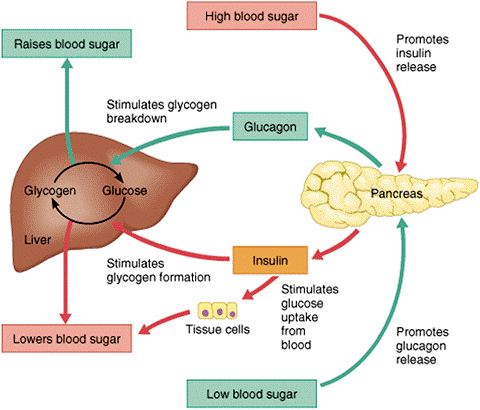
Diabetes mellitus (DM) refers to a group of metabolic diseases characterized by chronic hyperglycemia — elevated blood glucose — resulting from defects in insulin secretion, insulin action, or both. In children and adolescents, diabetes can present differently than in adults, with unique clinical features and implications for growth and development.
There are multiple forms of diabetes that may occur in children:
Type 1 Diabetes Mellitus (T1DM): Autoimmune destruction of pancreatic beta cells leading to absolute insulin deficiency—most common in children.
Type 2 Diabetes Mellitus (T2DM): Insulin resistance with relative insulin deficiency—previously rare in children but rising globally.
Monogenic diabetes and neonatal diabetes: Rare genetic causes.
Secondary diabetes: Due to other conditions like cystic fibrosis or steroid use.
T1DM is historically the dominant form in children, but T2DM is increasing in parallel with obesity and lifestyle changes.
2. Epidemiology
Understanding the global patterns of childhood diabetes helps guide screening, prevention, and resource allocation.
2.1 Global Incidence and Trends
Worldwide, the incidence of childhood diabetes has increased steadily over recent decades.
From 1990 to 2019, incident cases of childhood diabetes increased by about 39.4%, with the global incidence rate rising from 9.31 to 11.61 per 100,000 children.
The greatest increases occurred in children aged 10–14 years and in middle-income regions.
2.2 Type Distribution
T1DM accounts for 80–90% or more of pediatric diabetes globally.
T2DM among pediatric cases is smaller but growing rapidly in many countries, particularly where childhood obesity rates are climbing.
2.3 Regional Variability
Geography matters:
Rates vary widely, with Finland historically having some of the highest rates of pediatric T1DM (~30+ per 100,000).
Incidence is increasing significantly in low and middle-income countries, sometimes faster than in high-income regions.
3. Pathophysiology
Diabetes is not one disorder — it is a syndrome of hyperglycemia, and mechanisms differ:
3.1 Type 1 Diabetes
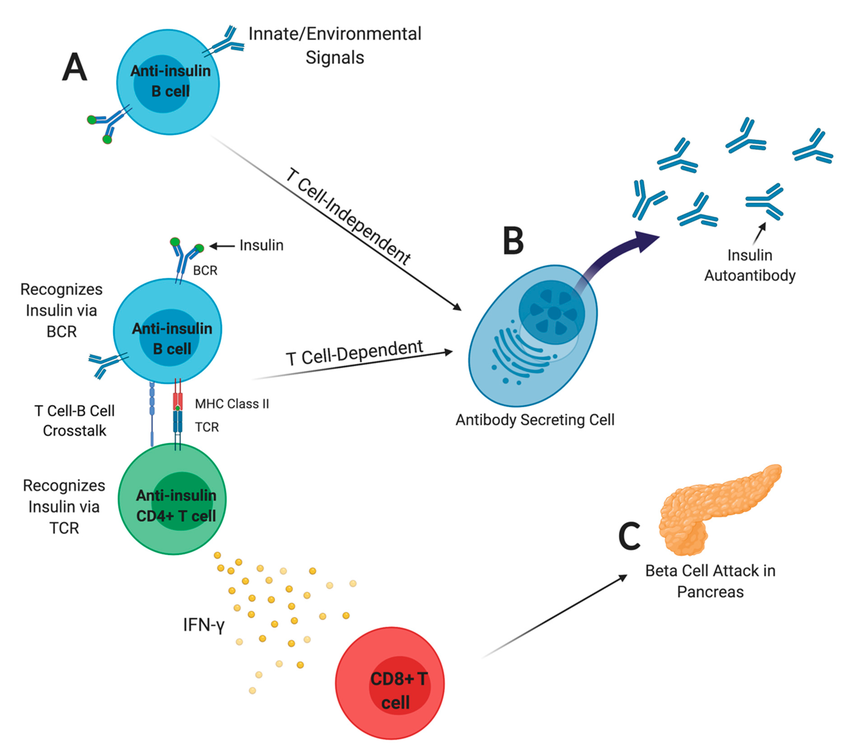
T1DM is caused by autoimmune destruction of pancreatic beta cells — the cells that produce insulin. Genetic predisposition plus environmental triggers (viral infections, early diet, etc.) are thought to provoke the autoimmune attack. The hallmark is an absolute lack of insulin.
Diagram Explanation: Beta cells in the islets of Langerhans are progressively destroyed by activated immune cells. Without insulin, glucose cannot enter tissues — leading to high blood glucose and energy starvation despite abundant glucose in the bloodstream.
3.2 Type 2 Diabetes
T2DM arises from insulin resistance — tissues fail to respond to insulin — initially compensated by increased insulin production, followed by beta-cell dysfunction.
In children, this is commonly linked to:
Obesity
Sedentary lifestyle
Genetic predisposition
T2DM typically presents in adolescents, often with features of metabolic syndrome (obesity, high lipids, high blood pressure).
4. Clinical Presentation
4.1 Common Symptoms
Diabetes symptoms often relate to high glucose levels and dehydration:
Polyuria (frequent urination)
Polydipsia (increased thirst)
Polyphagia (increased hunger) despite weight loss
Fatigue
Blurred vision
In young children, symptoms can be subtle or nonspecific. For T1DM, onset can be rapid.
4.2 Diabetic Ketoacidosis (DKA)
DKA is a life-threatening emergency, especially in T1DM:
Marked hyperglycemia (often > 250 mg/dL)
Ketone production
Metabolic acidosis
Dehydration
It presents with vomiting, abdominal pain, rapid breathing, and altered consciousness. Early recognition and immediate care save lives.
5. Diagnosis
Diagnosis is based on blood glucose measurements:
Fasting Plasma Glucose ≥ 126 mg/dL
Random Plasma Glucose ≥ 200 mg/dL + symptoms
HbA1c ≥ 6.5% (reflects average glucose over ~3 months)
For T1DM, autoantibody testing (e.g., GAD65, IA-2) may help confirm autoimmune etiology.
6. Management and Treatment
6.1 Type 1 Diabetes
There is no cure — treatment centers on insulin therapy:
Multiple daily injections or continuous subcutaneous insulin infusion (pump)
Frequent glucose monitoring (finger stick or CGM)
Nutrition planning
Physical activity adjustments
6.2 Type 2 Diabetes
Focuses on:
Lifestyle changes (diet, exercise)
Oral medications (e.g., metformin)
Insulin in some cases
Children with T2DM often need multidisciplinary care — involving dietitians, endocrinologists, and psychologists.
7. Complications
Long-term complications stem from chronic hyperglycemia:
7.1 Microvascular
Retinopathy (eye damage)
Nephropathy (kidney disease)
Neuropathy (nerve damage)
7.2 Macrovascular
Cardiovascular disease risk increases over time — even in youth with poorly controlled diabetes.
7.3 Acute Complications
Hypoglycemia (low blood glucose)
DKA
Both are preventable with good monitoring and education.
8. Growth, Development, and Adolescence
Children with diabetes face unique challenges:
Growth spurts alter insulin needs
Puberty induces insulin resistance
Peer dynamics influence adherence to management plans
Psychological support is essential.
9. Prevention and Public Health
9.1 Primary Prevention (T1DM)
Currently no proven method prevents T1DM onset. Research on immune modulation and early diet continues.
9.2 Preventing T2DM
This is actionable:
Promote healthy diet and physical activity
Reduce childhood obesity
Screen at-risk groups (family history, obesity)
Public campaigns and school programs are key.
10. Future Directions
Research themes include:
Immunotherapy to delay or prevent T1DM
Better artificial pancreas technologies
Genetic predictors of monogenic diabetes
11. Classification of Diabetes Mellitus in Children
Diabetes mellitus in children is a heterogeneous group of disorders, not limited to only type 1 and type 2 diabetes.
11.1 Type 1 Diabetes Mellitus
Autoimmune (Type 1A) – most common
Idiopathic (Type 1B) – no identifiable autoantibodies
Characterized by absolute insulin deficiency
11.2 Type 2 Diabetes Mellitus
Insulin resistance with relative insulin deficiency
Increasing prevalence in adolescents
Strong association with obesity and family history
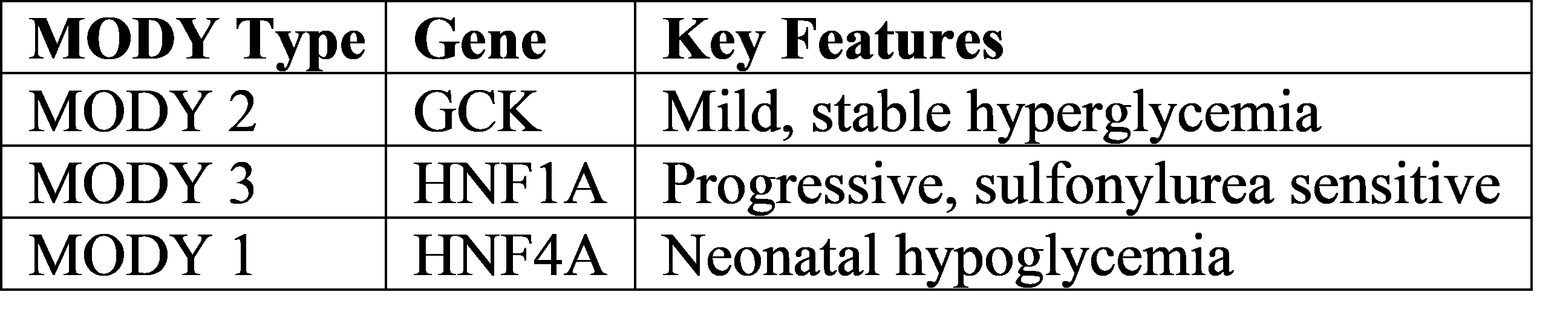
11.3 Monogenic Diabetes
Includes:
Maturity-Onset Diabetes of the Young (MODY)
Neonatal diabetes (onset before 6 months of age)
Important because some forms do not require insulin and respond to oral agents.
Table: Common MODY Types
11.4 Secondary Diabetes
Occurs due to:
Cystic fibrosis
Chronic pancreatitis
Endocrine disorders (Cushing syndrome)
Drug-induced (glucocorticoids, chemotherapy)
12. Genetic and Environmental Risk Factors
12.1 Genetic Susceptibility
Strong association with HLA class II genes (DR3, DR4, DQ2, DQ8)
Sibling risk: ~6–7%
Twin concordance: ~30–50%
12.2 Environmental Triggers
Proposed triggers include:
Viral infections (Coxsackie B, rubella)
Early exposure to cow’s milk proteins
Vitamin D deficiency
Gut microbiome alterations
These factors may initiate autoimmune beta-cell destruction in genetically predisposed children.
13. Pathogenesis of Diabetic Ketoacidosis (DKA)
DKA is a catabolic state caused by insulin deficiency and excess counter-regulatory hormones.
Pathophysiological Sequence
Absolute insulin deficiency
Increased glucagon, cortisol, catecholamines
Increased gluconeogenesis and lipolysis
Free fatty acids converted to ketone bodies
Metabolic acidosis + dehydration
14. Laboratory Evaluation in Pediatric Diabetes
14.1 Routine Investigations
Fasting and random blood glucose
HbA1c
Urine ketones
Serum electrolytes
14.2 Autoimmune Markers (T1DM)
Anti-GAD antibodies
Islet cell antibodies (ICA)
Insulin autoantibodies (IAA)
Anti-IA-2 antibodies
14.3 C-Peptide Levels
Low or absent → Type 1 DM
Normal or high → Type 2 or MODY
15. Nutritional Management in Children with Diabetes
Nutrition is not restrictive, but balanced and individualized.
15.1 Key Principles
Age-appropriate caloric intake
Consistent carbohydrate distribution
Avoid refined sugars
Encourage fiber-rich foods
15.2 Carbohydrate Counting
Allows flexible insulin dosing
Essential in intensive insulin therapy
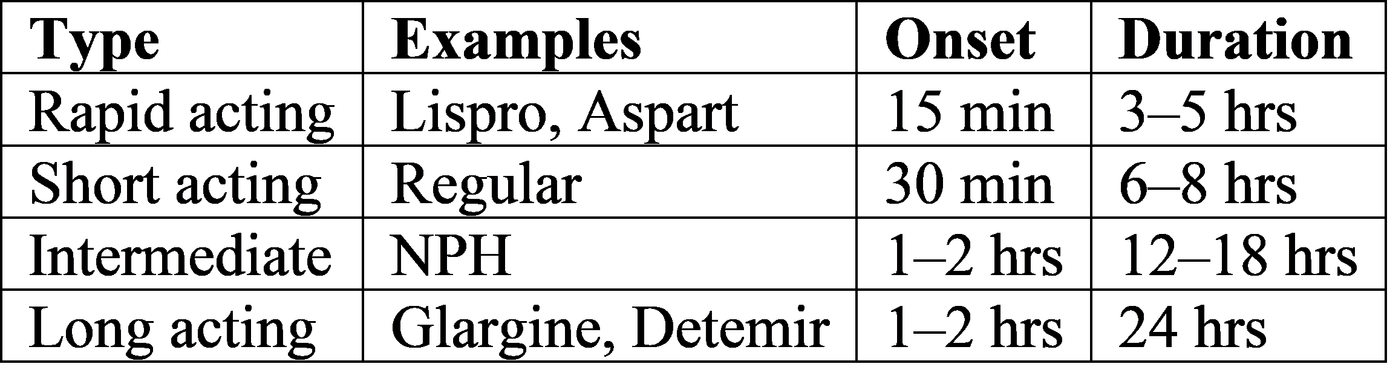
16. Insulin Therapy – Advanced Concepts
16.1 Types of Insulin
16.2 Insulin Delivery Methods
Syringes
Insulin pens
Insulin pumps
Hybrid closed-loop systems (artificial pancreas)
Continuous glucose monitoring (CGM) improves glycemic control and reduces hypoglycemia.
17. Hypoglycemia in Children with Diabetes
17.1 Causes
Excess insulin
Missed meals
Exercise without adjustment
17.2 Symptoms
Tremors
Sweating
Confusion
Seizures (severe cases)
17.3 Management
Oral glucose (15 g rule)
IV dextrose or glucagon injection for severe cases
18. Psychosocial Aspects of Pediatric Diabetes
Diabetes affects mental health, especially in adolescents.
Common Issues
Diabetes distress
Anxiety and depression
Eating disorders (diabulimia)
Poor adherence during adolescence
Psychological counseling is essential for long-term outcomes.
19. Diabetes and School Life
Schools must support children with diabetes:
Access to glucose monitoring
Permission to eat snacks
Emergency hypoglycemia management
Teacher awareness programs
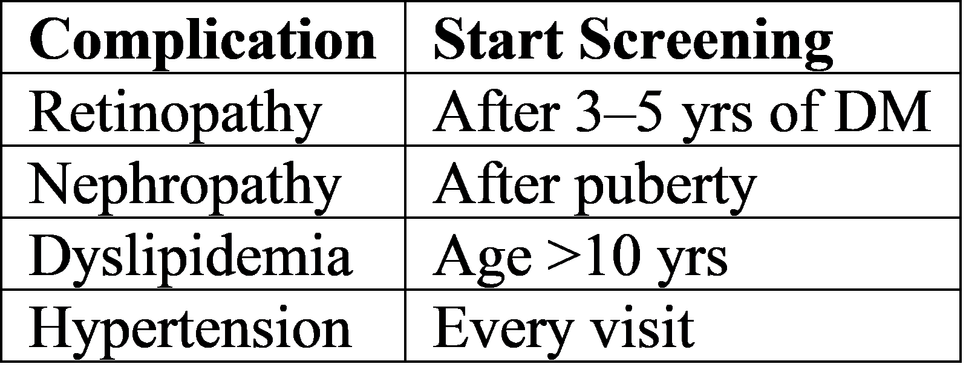
20. Screening and Follow-Up Protocols
Routine Screening Schedule
21. Recent Advances and Research
21.1 Immunotherapy
Teplizumab delays onset of T1DM in high-risk children
21.2 Artificial Pancreas Systems
Automated insulin delivery
Reduced glycemic variability
21.3 Stem Cell and Beta-Cell Replacement
Experimental but promising
22. Prognosis
With early diagnosis and optimal management:
Normal growth and development
Reduced complications
Near-normal life expectancy
Poor control leads to:
Early complications
Reduced quality of life
23. Conclusion
Diabetes mellitus in children is a lifelong condition requiring multidisciplinary care. Advances in insulin therapy, monitoring technologies, and education have dramatically improved outcomes. Early diagnosis, family support, psychological care, and public health strategies are critical to reducing morbidity and mortality. Prevention of type 2 diabetes through lifestyle interventions remains a major priority.
Reference
Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM.
Nelson Textbook of Pediatrics. 22nd ed. Philadelphia: Elsevier; 2024.
Chapter: Diabetes Mellitus in Children and Adolescents.Sperling MA.
Pediatric Endocrinology. 5th ed. Philadelphia: Elsevier; 2020.
Chapter 14: Diabetes Mellitus.Feingold KR, Anawalt B, Boyce A, et al., editors.
Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000–.
Available from: https://www.ncbi.nlm.nih.gov/books/Harrison’s Principles of Internal Medicine.
21st ed. New York: McGraw-Hill Education; 2022.
Section: Diabetes Mellitus.
American Diabetes Association (ADA).
Children and Adolescents: Standards of Medical Care in Diabetes—2024.
Diabetes Care. 2024;47(Suppl 1):S279–S301.
doi:10.2337/dc24-S014International Society for Pediatric and Adolescent Diabetes (ISPAD).
ISPAD Clinical Practice Consensus Guidelines 2022.
Pediatric Diabetes. 2022;23(Suppl 27):1–370.World Health Organization (WHO).
Classification of Diabetes Mellitus. Geneva: WHO; 2019.
Mayer-Davis EJ, et al.
Incidence Trends of Type 1 and Type 2 Diabetes among Youths.
New England Journal of Medicine. 2017;376:1419–1429.
doi:10.1056/NEJMoa1610187Patterson CC, et al.
Trends and Cycles in the Incidence of Childhood Type 1 Diabetes.
Diabetologia. 2019;62:408–417.
doi:10.1007/s00125-018-4763-3Dabelea D, et al.
Etiology and Pathophysiology of Type 2 Diabetes in Youth.
Diabetes Care. 2014;37(6):1563–1573.