Inflammatory Diseases of the Pelvic Organs: Bartholinitis, Vaginitis, Cervicitis, Endometritis, Pyometra, Salpingitis, Oophoritis, Parametritis, and Pelvic Abscess
1. Aydarbek Kyzy A.
2. Ayush Patil
3. Manas Kinge
4. Vishnu Saini
5. Aakash Dubey
6. Aaryan Patial
(Teacher, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
Abstract
Inflammatory diseases of the pelvic organs represent a significant proportion of gynecological morbidity worldwide, particularly among women of reproductive age. These conditions commonly arise from ascending infections of the lower genital tract and may involve multiple pelvic structures simultaneously. This review provides a comprehensive overview of major pelvic inflammatory conditions, including bartholinitis, vaginitis, cervicitis, endometritis, pyometra, salpingitis, oophoritis, parametritis, and pelvic abscess. The pathogenesis, clinical manifestations, diagnostic approaches, and current management strategies are discussed. Early recognition and timely treatment are essential to prevent severe complications such as infertility, chronic pelvic pain, ectopic pregnancy, and systemic sepsis.
Keywords
Pelvic inflammatory disease, Bartholinitis, Vaginitis, Cervicitis, Endometritis, Pyometra, Salpingitis, Oophoritis, Parametritis, Pelvic abscess, Gynecology
Introduction
Inflammatory diseases of the pelvic organs constitute a broad spectrum of infectious conditions affecting the female reproductive tract. These disorders often originate in the vagina or cervix and ascend to involve the uterus, fallopian tubes, ovaries, and surrounding pelvic tissues. The most common etiological agents include Chlamydia trachomatis, Neisseria gonorrhoeae, anaerobic bacteria, and mixed polymicrobial flora.
Pelvic inflammatory diseases (PID) are associated with substantial reproductive and obstetric complications. Delayed diagnosis and inadequate treatment may lead to irreversible damage to pelvic organs. Therefore, understanding the clinical features and management of individual inflammatory conditions is critical for effective gynecological care.
Bartholinitis
Bartholinitis is an inflammatory condition of the Bartholin glands, which are paired mucus-secreting glands located at the posterolateral aspect of the vaginal introitus. Their primary function is to provide lubrication to the vulva during sexual activity.
Pathophysiology
Bartholinitis is the inflammation of the Bartholin gland, usually resulting from obstruction of the duct and secondary bacterial infection. Common pathogens include Escherichia coli, Staphylococcus aureus, and sexually transmitted organisms.
Clinical Features
Painful swelling in the posterior labia majora
Dyspareunia
Fever in abscess formation
Difficulty walking or sitting
Management
Antibiotic therapy
Incision and drainage for abscess
Marsupialization in recurrent cases
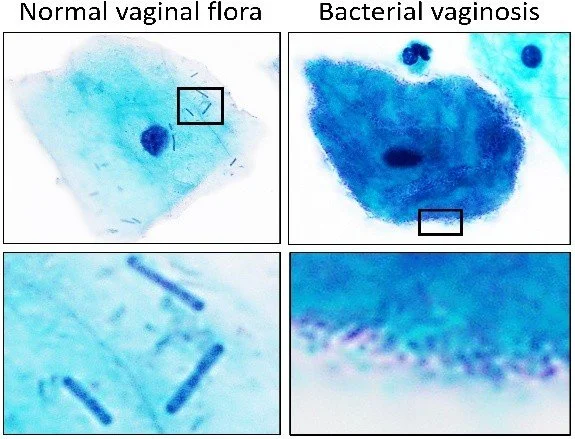
Vaginitis
Etiology
Bacterial vaginosis
Vulvovaginal candidiasis
Trichomoniasis
Clinical Features
Abnormal vaginal discharge
Pruritus and burning sensation
Vaginal odor
Dysuria or dyspareunia
Management
Antimicrobial or antifungal therapy based on etiology
Restoration of normal vaginal flora
Cervicitis
Pathophysiology
Cervicitis involves inflammation of the cervical epithelium, most commonly caused by sexually transmitted infections.
Clinical Features
Mucopurulent cervical discharge
Postcoital bleeding
Pelvic discomfort
Often asymptomatic
Management
Empirical antibiotic therapy
Partner treatment and STI screening
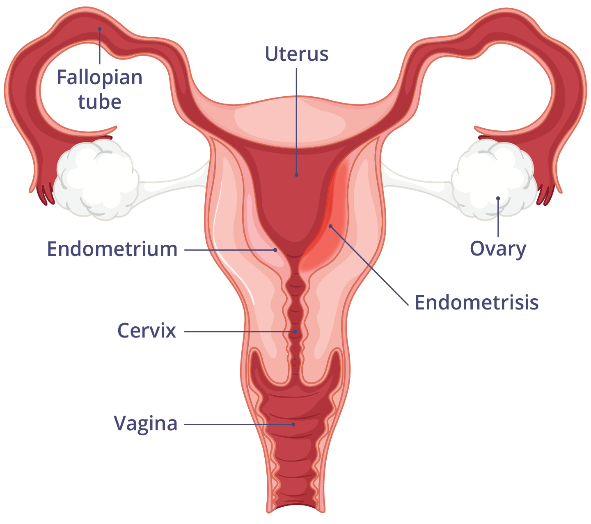
Endometritis
Pathophysiology
Endometritis is inflammation of the endometrial lining, commonly occurring postpartum or following gynecological procedures.
Clinical Features
Fever
Lower abdominal pain
Foul-smelling lochia or discharge
Uterine tenderness
Management
Broad-spectrum intravenous antibiotics
Supportive care
Pyometra
Pathophysiology
Pyometra is the accumulation of purulent material within the uterine cavity, often due to cervical obstruction.
Clinical Features
Postmenopausal bleeding
Lower abdominal pain
Fever and sepsis in severe cases
Management
Cervical dilation and drainage
Antibiotic therapy
Surgical intervention if complicated
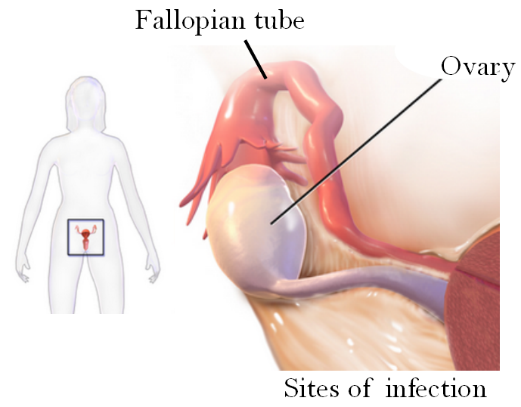
Salpingitis and Oophoritis
Pathophysiology
Salpingitis refers to inflammation of the fallopian tubes, while oophoritis involves the ovaries. These conditions often coexist as part of PID.
Clinical Features
Bilateral lower abdominal pain
Fever
Adnexal tenderness
Infertility in chronic cases
Management
Broad-spectrum antibiotics
Hospitalization in severe disease
Parametritis
Pathophysiology
Parametritis is inflammation of the connective tissue surrounding the uterus, often extending from endometritis.
Clinical Features
Pelvic pain
Fever
Pelvic mass in advanced cases
Management
High-dose antibiotics
Surgical drainage if abscess develops
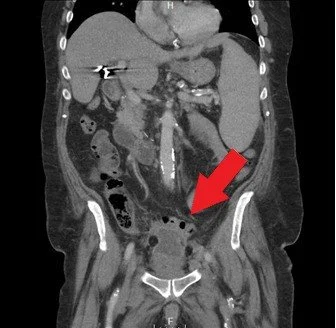
Pelvic Abscess
Pathophysiology
A pelvic abscess represents a localized collection of pus, commonly developing as a complication of untreated PID.
Clinical Features
Severe pelvic pain
High-grade fever
Signs of systemic infection
Management
Intravenous antibiotics
Image-guided drainage or surgery
Integrated Clinical Perspective
Inflammatory diseases of the pelvic organs are often interrelated, with infection spreading from one anatomical site to another. A syndromic approach to diagnosis and early initiation of treatment significantly reduces morbidity and long-term reproductive sequelae. Advances in imaging, microbiological diagnostics, and minimally invasive interventions have improved patient outcomes.
Conclusion
Inflammatory pelvic organ diseases remain a major challenge in gynecological practice due to their potential for serious reproductive and systemic complications. Early diagnosis, appropriate antimicrobial therapy, and preventive strategies such as sexual health education are essential. A multidisciplinary and patient-centered approach is vital to reducing disease burden and improving women’s reproductive health outcomes.
References
1. Mitchell C, et al. Pelvic inflammatory disease: Current concepts in diagnosis and management. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3843151/
2. Jennings LK. Pelvic Inflammatory Disease. StatPearls; 2023. https://www.ncbi.nlm.nih.gov/books/NBK499959/
3. Goje O. Pelvic Inflammatory Disease (PID). MSD Manual. https://www.msdmanuals.com/professional/gynecology-and-obstetrics/vaginitis-cervicitis-and-pelvic-inflammatory-disease/pelvic-inflammatory-disease-pid
4. CDC. PID Treatment Guidelines. https://www.cdc.gov/std/treatment-guidelines/pid.htm
5. Vaginitis, Cervicitis & PID. Mount Sinai research. https://scholars.mssm.edu/en/publications/vaginitis-cervicitis-and-pelvic-inflammatory-disease
6. Salpingitis (Fallopian Tube Inflammation). Wikipedia. https://en.wikipedia.org/wiki/Salpingitis
7. Cervicitis (Cervical Inflammation). Wikipedia. https://en.wikipedia.org/wiki/Cervicitis