Neuroendocrine Syndromes in Gynecology: Asherman Syndrome, Galactorrhea–Amenorrhea, Sheehan Syndrome, and Adrenogenital
1. Aydarbek Kyzy A.
2. Akhilesh Yadav
3. Virochan Kumar Giri
4. Tushar Jain
5. Sarfaraz Hussain
6. Shubham Verma
(Teacher, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
(Student, International Medical Faculty, Osh State University, Kyrgyzstan)
Abstract
Neuroendocrine regulation plays a pivotal role in maintaining normal female reproductive physiology. Disruption of the hypothalamic–pituitary–ovarian–adrenal axis can result in a spectrum of gynecological disorders with systemic implications. This review examines key neuroendocrine syndromes relevant to gynecological practice, including Asherman syndrome, galactorrhea–amenorrhea syndrome, Sheehan syndrome, and adrenogenital syndromes. Each condition is explored in terms of pathophysiology, clinical presentation, diagnostic strategies, and contemporary management. Understanding these disorders is essential for early diagnosis, prevention of long-term complications such as infertility and metabolic disturbances, and optimization of reproductive health outcomes.
Keywords
Neuroendocrine disorders, Asherman syndrome, Galactorrhea–amenorrhea, Sheehan syndrome, Adrenogenital syndrome, Hypothalamic–pituitary axis, Gynecology
Introduction
The female reproductive system is intricately regulated by neuroendocrine pathways involving the hypothalamus, pituitary gland, ovaries, and adrenal glands. Hormonal feedback mechanisms ensure cyclic ovulation, menstruation, and fertility. Disturbances in these pathways can lead to complex gynecological syndromes with endocrine, reproductive, and psychological consequences.
Neuroendocrine syndromes in gynecology often present with menstrual irregularities, infertility, galactorrhea, and virilization. Their multifactorial etiology requires a multidisciplinary approach integrating gynecology, endocrinology, and reproductive medicine.
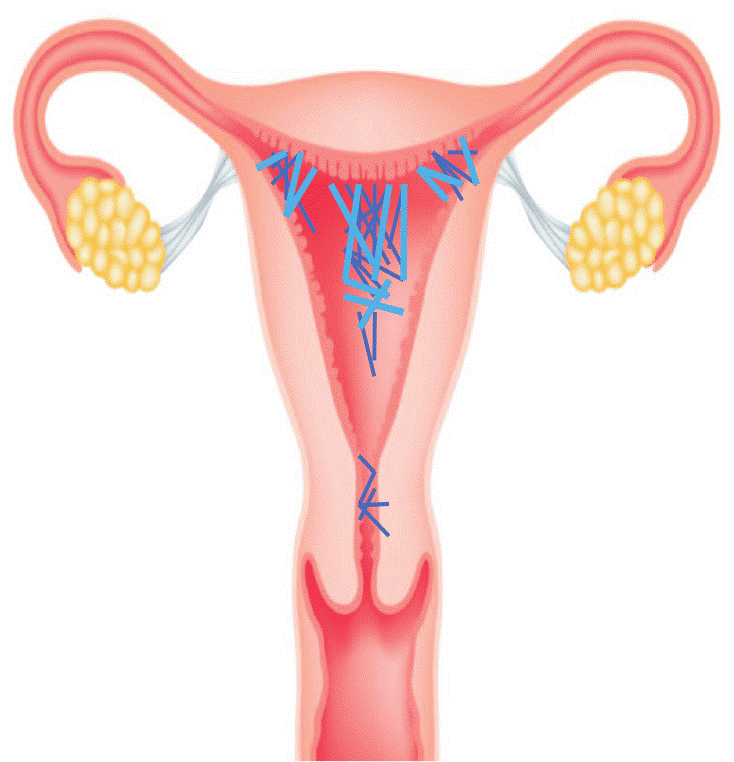
Asherman Syndrome
Pathophysiology
Asherman syndrome is characterized by intrauterine adhesions resulting from endometrial trauma, most commonly following dilation and curettage after miscarriage or postpartum hemorrhage. The damage disrupts endometrial regeneration, leading to fibrosis and obliteration of the uterine cavity.
Clinical Features
Secondary amenorrhea or hypomenorrhea
Infertility and recurrent pregnancy loss
Cyclic pelvic pain due to outflow obstruction
Diagnosis
Hysteroscopy (gold standard)
Hysterosalpingography
Transvaginal ultrasound with saline infusion
Management
Hysteroscopic adhesiolysis
Postoperative estrogen therapy to promote endometrial healing
Use of intrauterine devices or balloons to prevent re-adhesion
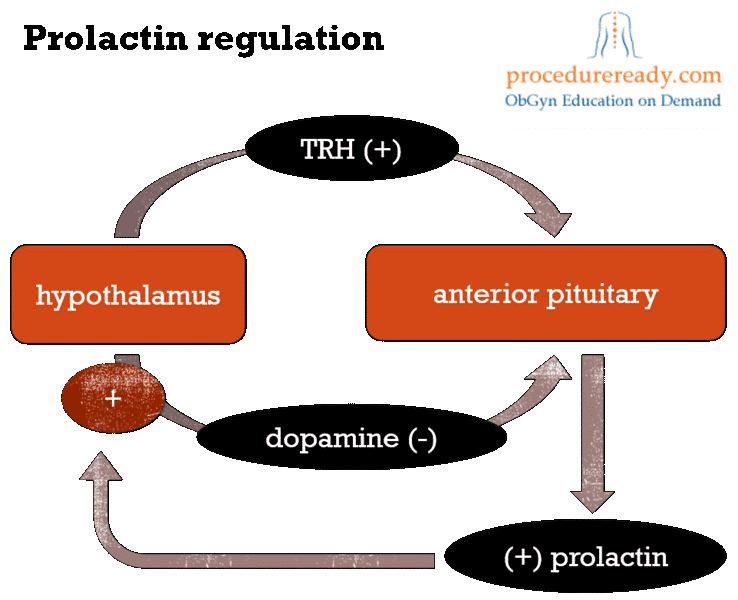
Galactorrhea–Amenorrhea Syndrome
Pathophysiology
This syndrome is most commonly caused by hyperprolactinemia, which suppresses gonadotropin-releasing hormone (GnRH), leading to decreased luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion.
Etiology
Pituitary adenomas (prolactinomas)
Hypothyroidism
Dopamine antagonist medications
Clinical Features
Galactorrhea unrelated to lactation
Amenorrhea or oligomenorrhea
Infertility and decreased libido
Management
Dopamine agonists (bromocriptine, cabergoline)
Treatment of underlying causes
Surgical intervention in resistant cases
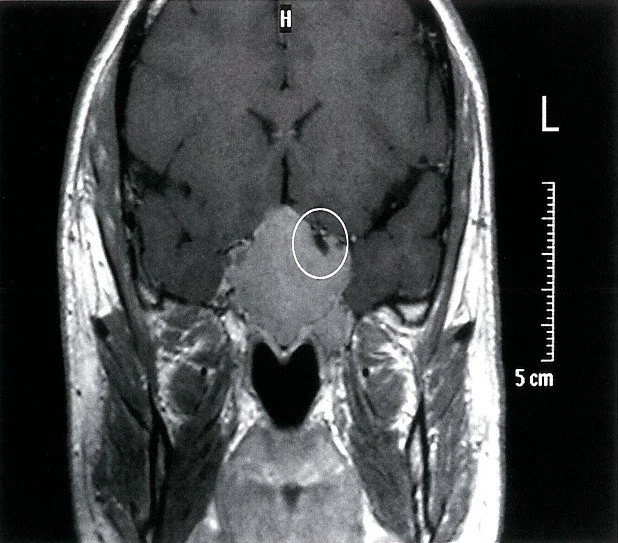
Sheehan Syndrome
Pathophysiology
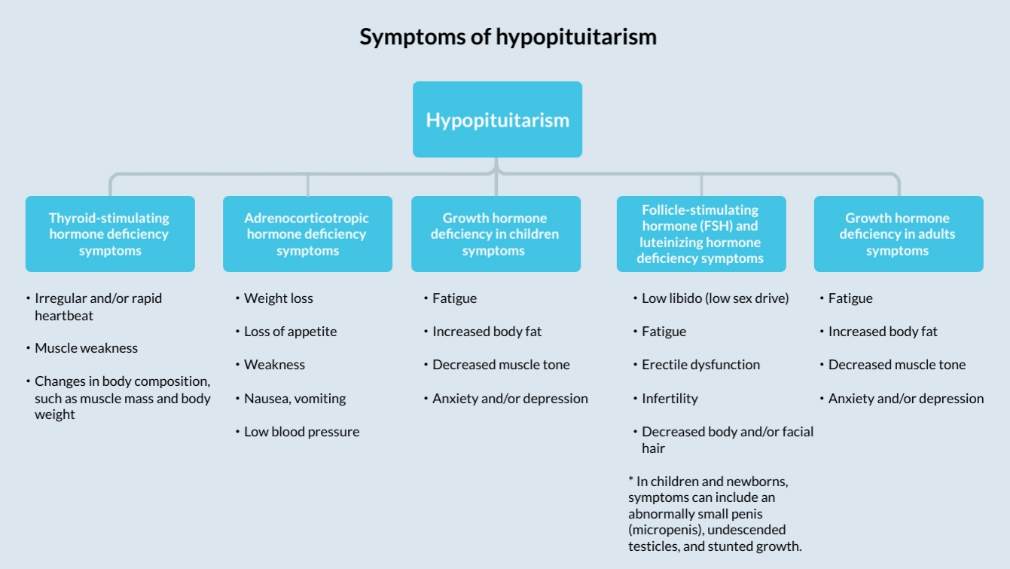
Sheehan syndrome results from ischemic necrosis of the pituitary gland following severe postpartum hemorrhage. The enlarged pituitary during pregnancy is particularly vulnerable to hypovolemia.
Clinical Features
Failure of lactation postpartum
Amenorrhea
Fatigue, hypotension, hypothyroidism
Secondary adrenal insufficiency
Diagnosis
Low pituitary hormone levels
MRI showing pituitary atrophy
Management
Lifelong hormone replacement therapy
Glucocorticoids, thyroid hormones, estrogen–progesterone therapy
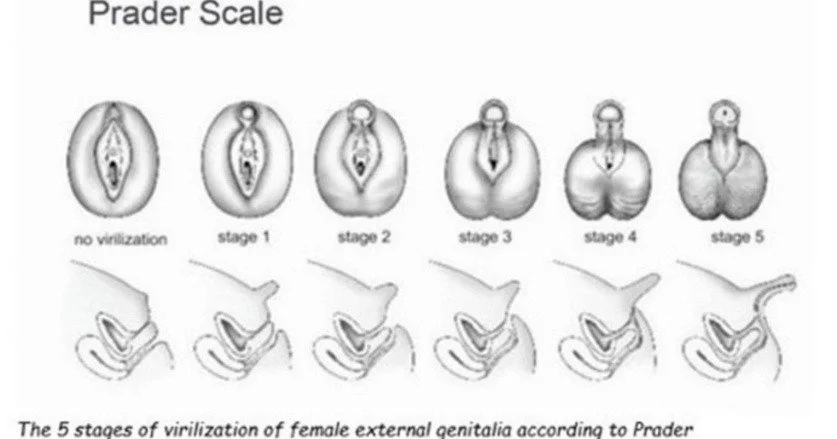
Adrenogenital Syndromes
Pathophysiology
Adrenogenital syndromes are caused by enzymatic defects in adrenal steroid synthesis, most commonly 21-hydroxylase deficiency, leading to excess androgen production.
Clinical Features
Virilization in females
Ambiguous genitalia at birth
Precocious puberty or menstrual irregularities
Diagnosis
Elevated adrenal androgens
ACTH stimulation test
Genetic testing
Management
Glucocorticoid therapy to suppress androgen excess
Surgical correction when necessary
Fertility counseling
Integrated Neuroendocrine Perspective
These syndromes demonstrate the profound interdependence of endocrine and reproductive systems. Early recognition prevents irreversible complications such as infertility, metabolic disorders, and psychological distress. Advances in imaging, hormonal assays, and minimally invasive surgery have significantly improved outcomes.
Conclusion
Neuroendocrine syndromes in gynecology represent complex disorders requiring comprehensive evaluation and long-term management. Asherman syndrome, galactorrhea–amenorrhea syndrome, Sheehan syndrome, and adrenogenital syndromes exemplify how hormonal dysregulation can profoundly impact female reproductive health. A multidisciplinary and patient-centered approach is essential for early diagnosis, effective treatment, and improved quality of life.
References
1. Melmed S, Polonsky KS, Larsen PR, Kronenberg HM: Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.elsevier.com/books/williams-textbook-of endocrinology/9780323297387
2. Hoffman BL, Schorge JO, Bradshaw KD, et al.: Williams Gynecology. 4th ed. McGraw-Hill; 2020. https://accessmedicine.mhmedical.com/book.aspx?bookID=2658
3. Speroff L, Fritz MA: Clinical Gynecologic Endocrinology and Infertility. 9th ed. Lippincott Williams & Wilkins; 2020. https://shop.lww.com/Clinical-Gynecologic-Endocrinology-and-Infertility/p/9781451185614
4. Asherman JG: Amenorrhoea traumatica (atretica). Journal of Obstetrics and Gynaecology of the British Empire. 1948. https://pubmed.ncbi.nlm.nih.gov/18867505/
5. Yu D, Wong YM, Cheong Y, Xia E, Li TC: Asherman syndrome—one century later. Fertility and Sterility. 2008;89(4):759–779. https://pubmed.ncbi.nlm.nih.gov/18339378/
6. Molitch ME: Diagnosis and treatment of pituitary adenomas. JAMA. 2017;317(5):516–524. https://jamanetwork.com/journals/jama/fullarticle/2603494
7. Biller BMK, Luciano A, Crosignani PG, et al.: Guidelines for the diagnosis and treatment of hyperprolactinemia. Journal of Clinical Endocrinology & Metabolism. 1999. https://academic.oup.com/jcem/article/84/10/3859/2864526
8. Kleinberg DL, Noel GL, Frantz AG: Galactorrhea: a study of 235 cases. New England Journal of Medicine. 1977. https://www.nejm.org/doi/full/10.1056/NEJM197703172961101
9. Kelestimur F.: Sheehan’s syndrome. Pituitary. 2003;6(4):181–188. https://pubmed.ncbi.nlm.nih.gov/14674704/
10. Karaca Z, Laway BA, Dokmetas HS, Kelestimur F.: Sheehan syndrome. Nature Reviews Disease Primers. 2016. https://www.nature.com/articles/nrdp201692
11. Bornstein SR, Allolio B, Arlt W, et al.: Diagnosis and treatment of primary adrenal insufficiency. JCEM. 2016. https://academic.oup.com/jcem/article/101/2/364/2804869
12. Speiser PW, Arlt W, Auchus RJ, et al.: Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. JCEM. 2018. https://academic.oup.com/jcem/article/103/11/4043/5070382
13. Forest MG: Adrenogenital syndrome. Baillière’s Clinical Endocrinology and Metabolism. 1991. https://pubmed.ncbi.nlm.nih.gov/2050424/
14. New MI.: Nonclassical 21-hydroxylase deficiency. JCEM. 2006. https://pubmed.ncbi.nlm.nih.gov/17018651/
15. American Society for Reproductive Medicine (ASRM): Uterine factor infertility. Fertility and Sterility. 2015. https://www.asrm.org/practice-guidance/practice-committee-documents/uterine-factor-infertility/