Polycystic Ovarian Syndrome
1. Thiyagarajan Sakhana
2. Um E Rumana
3. Appadurai Subashree
4. Aidarbek Kyzy Aidanek
(1,2,3. Student, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.
4. Teacher, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.)
INTRODUCTION
PCOD, or Polycystic Ovarian Disease, occurs when the ovaries produce immature or partially mature eggs, which can form cysts over time. This condition leads to hormonal imbalances but is generally less severe than PCOS.
Key Symptoms of PCOD
● Irregular menstrual cycles
● Weight gain
● Acne and oily skin
● Hair thinning
● Fatigue
CAUSES
PCOS can be caused by a variety of factors
While the exact causes of PCOS are currently unknown, research has found some common factors that may increase your risk. These include:
High levels of androgen hormones — Often associated with “male” hormones, androgens are a category of hormones that naturally occurs in both men and women. Higher levels of androgen hormones in females can lead to the development of PCOS and disrupt the normal function of the ovaries. Symptoms might include not ovulating releasing an egg) regularly during menstrual cycles, or having acne or extra hair growth on the face.
Elevated body weight and insulin resistance — Insulin is the main hormone responsible for controlling blood sugar levels, and insulin resistance is the second most common cause associated with developing PCOS. Insulin resistance is when your blood sugar levels are higher than normal, but not quite so high they fit a diagnosis for diabetes — this state may also be referred to as “pre-diabetes.” Women with PCOS may also have deposits of fat in their midsection. These fat cells are more likely to be resistant to insulin, causing the body to produce more insulin, causing blood sugar control problems and the possibility of developing type 2 diabetes. Insulin resistance can result in PCOS symptoms such as irregular periods, weight gain, higher levels of testosterone, and fertility problems.
Genetic and metabolic factors — There is a greater risk for PCOS when genetics and family history are a factor. While more research needs to examine the nature of the relationship between genetics and PCOS, women whose mothers, aunts, or grandmothers have had PCOS are more likely to develop the disease themselves.
PATHOPHYSIOLOGY
Hyperandrogenism is the most characteristic feature of PCOS, and some argue that it is the defining feature of the disease.
Hyperandrogenism is exacerbated by hyperinsulinemia and antral follicle arrest and may itself increase the risk of follicle arrest.
Similar ovarian characteristics have been noted in women with other conditions of androgen excess such as congenital adrenal hyperplasia.
Neuroendocrine abnormalities
Women with PCOS have an increase in the frequency of GnRH pulses; shorter pulses preferentially promote the production of luteinizing hormone (LH) and result in a decrease in the production of follicle stimulating hormone (FSH).
Patients with PCOS often exhibit an increase in the LH:FSH ratio, which may contribute to the ovarian excess of androgens relative to estrogens.
It is unclear if patients with PCOS have an intrinsically faster GnRH pulsation mechanism which initiates hyperandrogenism in the ovaries, or if oligoanovulation itself promotes more rapid pulsations in GnRH via a reduction in circulating progesterone.
Normally, progesterone is released from the corpus luteum following ovulation
Progesterone acts to slow GnRH pulsation
In PCOS, a decrease in ovulatory events may cause a decrease in circulating progesterone
Exposure to androgens in utero or prepubertally may decrease the inhibitory effects of estrogen and progesterone on the hypothalamus and contribute to increased pulsatility, Insulin resistance and T2DM 50-70% of patients with PCOS exhibit metabolic abnormalities, including poor glucose tolerance and hyperinsulinemia This is not solely a consequence of increased visceral obesity; rather, obesity and hormonal abnormalities are thought to make additive contributions to insulin resistance:
Patients with PCOS exhibit a greater degree of insulin resistance than patients with the same BMI and visceral adiposity who do not have PCOS
Functional insulin resistance is considered a consequence of defects in insulin-mediated glucose transport and signaling in adipocytes and myocytes; this may be the result of a dysregulation in adipokine production and signaling from adipose tissues but the mechanism is incompletely understood
The resulting hyperinsulinemia leads to insulin spillover into other tissues, most commonly the skin. Insulin acts via insulin-like growth factor receptors to cause excess keratinocyte growth, producing velvety skin patches known as acanthosis nigricans.
Polycystic ovaries are present in 20-30% of women and are not essential for the diagnosis of PCOS
The “cysts” in polycystic ovaries are not true cysts, but rather antral follicles which have arrested in development
This is thought to occur because of hormonal abnormalities:
Hyperandrogenism: arrest occurs when the granulosa cells of the ovaries normally begin to produce estrogen by aromatizing androstenedione produced by the theca cells; excess 5a-reduced androgens in the ovaries are thought to inhibit the action of aromatase and therefore reduce estradiol synthesis, which is required for further maturation
Hyperinsulinemia: exacerbates ovarian hyperandrogenism by (1) increasing 17a-hydroxylase activity in theca cells and promoting androstenedione and testosterone production; (2) promoting LH- and IGF1-stimulated androgen production; and (3) elevating free testosterone by decreasing the production of sex hormone binding globulin (SHBG)
SYMPTOMS AND SIGNS OF PCOS
Symptoms of PCOS typically begin during puberty and worsen with time. Ovulatory dysfunction is usually present at puberty, sometimes resulting in primary amenorrhea. Premature adrenarche is common, caused by excess dehydroepiandrosterone sulfate (DHEAS) and often characterized by early growth of axillary hair, body odor, and microcomedonal acne.
Typical symptoms include irregular menses (oligomenorrhea or amenorrhea); fertility is impaired in many patients. Other common symptoms are mild obesity and mild hirsutism. However, in up to half of women with PCOS, weight is normal, and some women are underweight.
Body hair may grow in a male pattern (eg, on the upper lip, chin, back, thumbs, and toes; around the nipples; and along the linea alba of the lower abdomen). Some women develop acne. Virilization (clitoromegaly, deepening of the voice, increased muscle mass, male pattern baldness, breast atrophy) suggests more severe hyperandrogenism (adrenal hyperandrogenism, androgen-secreting tumor).
Areas of thickened, darkened skin (acanthosis nigricans) may appear in the axillae, on the nape of the neck, in skinfolds, and on knuckles and/or elbows; the cause is high insulin levels due to insulin.
DIAGNOSIS OF PCOD
Clinical criteria
Hormone blood tests for androgens and to exclude other endocrinologic disorders, such as measurement of serum testosterone, follicle-stimulating hormone (FSH), prolactin, and thyroid-stimulating hormone (TSH) levels
Pelvic ultrasound
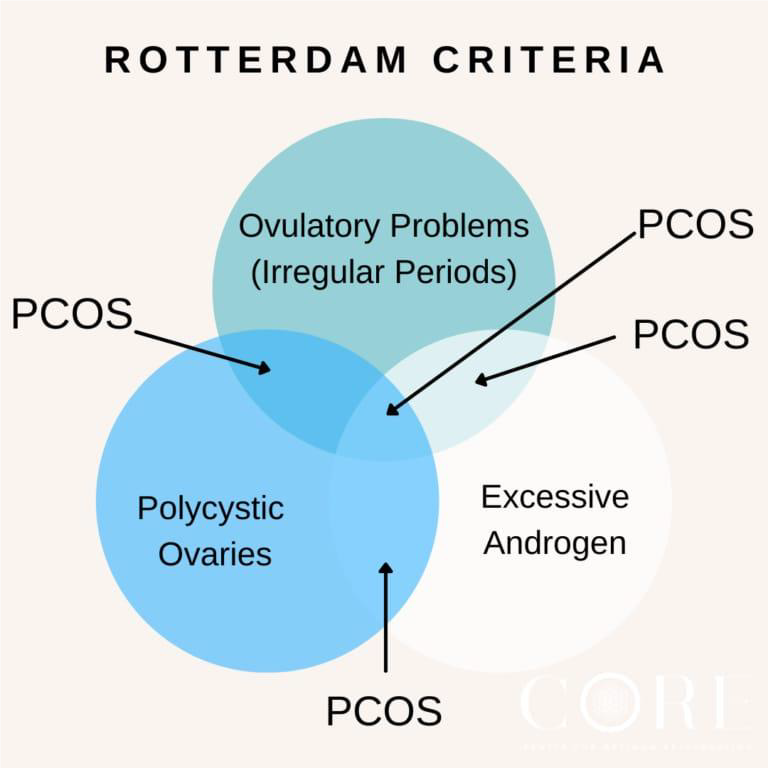
Diagnosis of PCOS is usually made based on the Rotterdam criteria, which requires at least 2 of the following 3 findings (1):
Oligo-ovulation and/or anovulation
Clinical and/or biochemical evidence of hyperandrogenism Polycystic ovaries (transvaginal ultrasound with 12 or more follicles in each ovary measuring 2 to 9 mm in diameter, and/or increased ovarian volume [>10 ml])
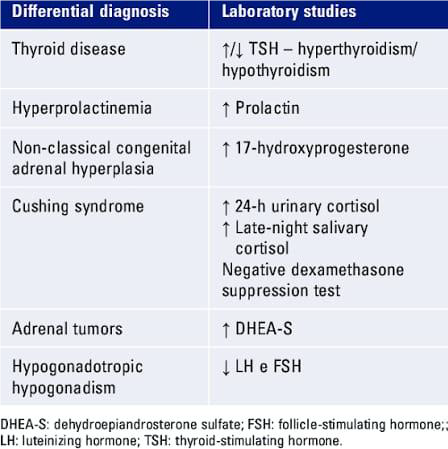
Blood tests include measurement of testosterone, which may be mildly elevated in PCOS; levels > 150 ng/dL suggest an ovarian or adrenal androgen-secreting tumor. Serum free testosterone is more sensitive than total testosterone but is technically more difficult to measure.
For patients with hirsutism or virilization, other etiologies of hyperandrogenism should be excluded by measuring other serum androgens including
Early-morning serum 17-hydroxyprogesterone to exclude adrenal hyperandrogenism
DHEAS; high levels (> 800 mcg/dL) suggest an adrenal androgen-secreting tumor
Testing includes pregnancy testing and measurement of FSH, prolactin, and TSH to exclude other possible causes of symptoms. Also, serum cortisol is measured to exclude Cushing syndrome, which may cause oligomenorrhea, hirsutism, and obesity.
Transvaginal ultrasound is done to detect polycystic ovaries and exclude other possible causes of symptoms. However, transvaginal ultrasound is not done in adolescent girls.
Complications
Complications of PCOS can include:
1. Infertility
2. Gestational diabetes or pregnancy-induced high blood pressure
3. Miscarriage or premature birth
4. Nonalcoholic steatohepatitis — a severe liver inflammation caused by fat buildup in the liver
Metabolic syndrome — a cluster of conditions including high blood pressure, high blood sugar, and unhealthy cholesterol or triglyceride levels that significantly increase your risk of heart and blood vessel (cardiovascular) disease
● Type 2 diabetes or prediabetes
● Sleep apnea
● Depression, anxiety and eating disorders
● Cancer of the uterine lining (endometrial cancer)
● Obesity commonly occurs with PCOS and can worsen complications of the disorder.
Having PCOS can increase your chance of having complications during pregnancy, such as:
● high blood pressure and pre-eclampsia
● gestational diabetes
● miscarriage
● premature birth
● caesarean birth
If you have PCOS, your baby may be larger than usual for their gestational age. This makes it more likely that you will need a caesarean birth.
Babies born to people with PCOS also have a higher chance of being admitted to a newborn intensive care unit.
If you have PCOS and are pregnant, it's important you talk to your doctor. You can reduce the chances of these pregnancy complications by:
● monitoring your PCOS symptoms
● taking extra care during your pregnancy
● Some women with PCOS may also develop type 2 diabetes after pregnancy.
SURGICAL MANAGEMENT
If you have tried lifestyle changes and medical treatments and they have not worked, surgery might be an option. This includes:
Laparoscopic ovarian surgery — this can help your ovaries work better and may restart or improve ovulation. During this keyhole surgery, the tissue in your ovaries that makes extra androgen hormones is removed.
Assisted reproductive technology — which is an option if other treatments have not worked. This technology works better for women who have made lifestyle changes and are a healthy weight before starting treatment.
1. Anxiety
Women with PCOS are more likely to suffer from anxiety. Concerns about fertility, irregular cycles, and changes in physical appearance can cause persistent worry and stress, which may interfere with daily life.
2. Depression
Depression is a common challenge among women with PCOS. Struggles with symptoms like acne, excess hair growth, or difficulty conceiving often contribute to feelings of sadness, hopelessness, and isolation.
3. Poor Self-Esteem
Visible symptoms of PCOS can take a toll on self-image. Weight fluctuations, hair growth, and skin problems may negatively affect self-confidence, leading to low self-esteem and social withdrawal, Psychological problems.
PREVENTION :
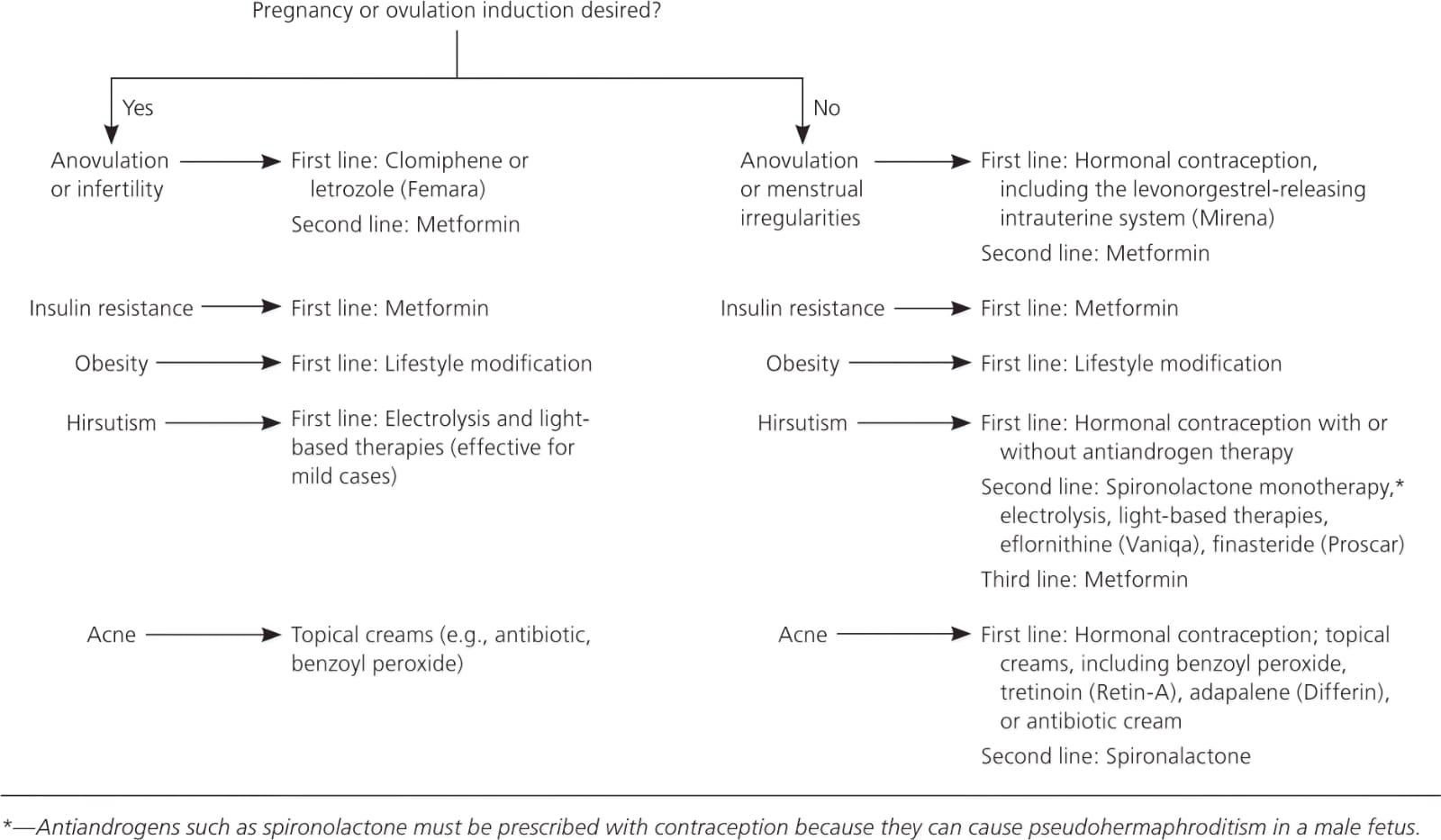
Lifestyle Modifications (First-Line Treatment): This is the cornerstone of PCOS management.Focus on a diet rich in fruits, vegetables, lean proteins, and whole grains while reducing intake of processed foods and high-sugar items. Adopting a low glycemic index (GI) diet can help manage insulin resistance.Aim for a minimum of 150 minutes of moderate-intensity activity (e.g., brisk walking, cycling) or 75 minutes of vigorous activity per week, including muscle-strengthening exercises.Losing even a modest 5% to 10% of body weight can significantly improve hormonal balance, insulin sensitivity, and menstrual regularity. Smoking increases the risk of heart disease and should be avoided.Counselling is an integral part of comprehensive PCOS care, addressing the significant psychosocial impact of the condition.
Emotional and Mental Health Support: Women with PCOS are at a higher risk of anxiety, depression, and body image issues due to symptoms like weight gain, acne, and hair growth.
Routine screening for anxiety and depressive symptoms is recommended at diagnosis and during follow-up appointments.
Psychological therapies, such as cognitive behavioral therapy (CBT), can be effective in managing mental health challenges.
Nutritional Counselling: Consulting a registered dietitian can provide personalized, evidence-based dietary plans that address individual symptoms and help achieve sustainable lifestyle changes.
Peer Support: Connecting with others who have PCOS through support groups can alleviate distress and improve self-management by providing a shared sense of experience and community.
Patient Education: Healthcare professionals should provide high-quality, culturally appropriate information to empower women to understand their condition and participate actively in their own care plans.
Multidisciplinary Care: Optimal management often involves a team of healthcare providers, including general practitioners, endocrinologists, dietitians, and mental health specialists, to address all facets of the condition.
Recent advances in PCOS focus on personalized care, new drugs (like SGLT-2 inhibitors, GLP-1 agonists), combination therapies (metformin + sitagliptin), microbiome-targeted treatments (probiotics), and recognizing PCOS as a lifelong metabolic condition, moving beyond just reproductive symptoms to include genetics, metabolism, and inflammation for proactive management with lifestyle, supplements (inositol), and precision medicine.
PCOS is a complex hormonal, metabolic, and psychological disorder with numerous clinical presentations. It is one of the most common reasons for infertility. Before contemplating any pharmaceutical options, lifestyle changes should be considered the primary therapeutic prescription for PCOS-related infertility. According to current research, PCOS increases the risk of endometrial cancer in women of all ages, although it has no effect on the risk of ovarian or breast cancer. These findings point to the possibility of gynaecological cancer morbidity as a result of PCOS.
CONCLUSION
Ovulation stimulation, which is best performed with letrozole, is the next phase, followed by CC. Gonadotropins were the next step for women who had failed first-line oral ovulatory medication. Pregnant women who do not use ovulation stimulants or who are experiencing other infertility issues may benefit from ART. Metformin in combination with CC or gonadotropin and as an adjuvant to IVF ICSI remains the best option for people with RI or hyperinsulinemia. While inositol and vitamin D may be beneficial to one's health, further study and advice are required. There is no clear proof of the efficacy of alternative treatments. Although insulin sensitizers such as metformin have long been used to treat PCOS metabolic dysfunctional, newer medicines such as incretin mimetics and SGLT2 inhibitors have proven to be more effective at reducing weight.