Thyroid and Parathyroid Glands
1. Manas Kyzy Uulkan
2. Suryansh Kushwaha
Pratham Parmar
(1. Lecturer, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic
2. Students, International Medical Faculty, Osh State University, Osh, Kyrgyz Republic.)
Abstract
The thyroid and parathyroid glands are closely related endocrine organs that play essential roles in metabolic regulation and calcium homeostasis. Despite their anatomical proximity, these glands differ significantly in embryological origin, histological organization, cellular composition, and hormonal function. Histological evaluation of these glands provides critical insights into their physiological roles and forms the foundation for diagnosing a wide spectrum of endocrine disorders. This review aims to present a comprehensive histology-focused analysis of the thyroid and parathyroid glands, emphasizing microscopic architecture, cellular morphology, staining characteristics, and structure–function relationships. A narrative literature review was conducted using peer-reviewed histology and pathology sources published between 2015 and 2024. The findings highlight the thyroid gland’s follicular organization, colloid dynamics, and distinct follicular and parafollicular cell populations, contrasted with the parathyroid gland’s solid cellular arrangement dominated by chief cells and oxyphil cells. Quantitative comparisons of cellular proportions and age-related histological changes are presented using pie charts and comparative graphs. Understanding these microscopic features is clinically significant for interpreting biopsy specimens, identifying pathological alterations, and correlating histological findings with endocrine dysfunction. This review reinforces the importance of histology as a cornerstone of endocrine diagnosis and medical education.
Keywords: Thyroid gland; Parathyroid gland; Histology; Follicular cells; Chief cells; Endocrine microscopy; Calcium homeostasis
Introduction
The thyroid and parathyroid glands are vital components of the endocrine system, regulating fundamental physiological processes including metabolism, growth, development, and mineral balance. Although anatomically adjacent in the anterior neck, these glands exhibit marked differences in microscopic organization and functional specialization. Histological examination remains the gold standard for understanding their normal structure and for identifying pathological alterations that underlie endocrine disease.
The thyroid gland primarily regulates basal metabolic rate through the secretion of thyroxine (T4) and triiodothyronine (T3), while the parathyroid glands maintain calcium and phosphate balance via parathyroid hormone (PTH). These hormonal functions are directly reflected in their cellular architecture, vascular supply, and stromal composition. Histology therefore provides a direct link between microscopic structure and physiological function.
Current medical education and diagnostic pathology emphasize the importance of recognizing normal histological patterns to differentiate them from pathological states such as thyroiditis, goiter, adenomas, and hyperparathyroidism. However, integrated histology-based comparisons of the thyroid and parathyroid glands are often underrepresented in the literature.
Aim
Describe the normal histological architecture of the thyroid and parathyroid glands
Compare cellular composition and organization using histology-based data
Correlate microscopic features with physiological and clinical significance
Methodology
Study Design
This study is a narrative histological literature review.
Data Sources
Peer-reviewed articles, histology atlases, and endocrine pathology textbooks published between 2015 and 2024 were reviewed using PubMed, Scopus, and Google Scholar.
Inclusion Criteria
● Studies focusing on normal histology of thyroid and/or parathyroid glands
● Articles emphasizing microscopy, staining, and cellular morphology
● Human histological studies
Exclusion Criteria
● Animal-only studies
● Pure biochemical or genetic studies without histological correlation
● Case reports lacking microscopic detail
Data Extraction
Data were extracted on:
● Cellular composition
● Tissue architecture
● Staining characteristics
● Functional histological variations
● Age-related changes
Ethical Considerations
This review utilized published data only and did not involve human or animal experimentation, thus ethical approval was not required.
Histological Overview of the Thyroid Gland
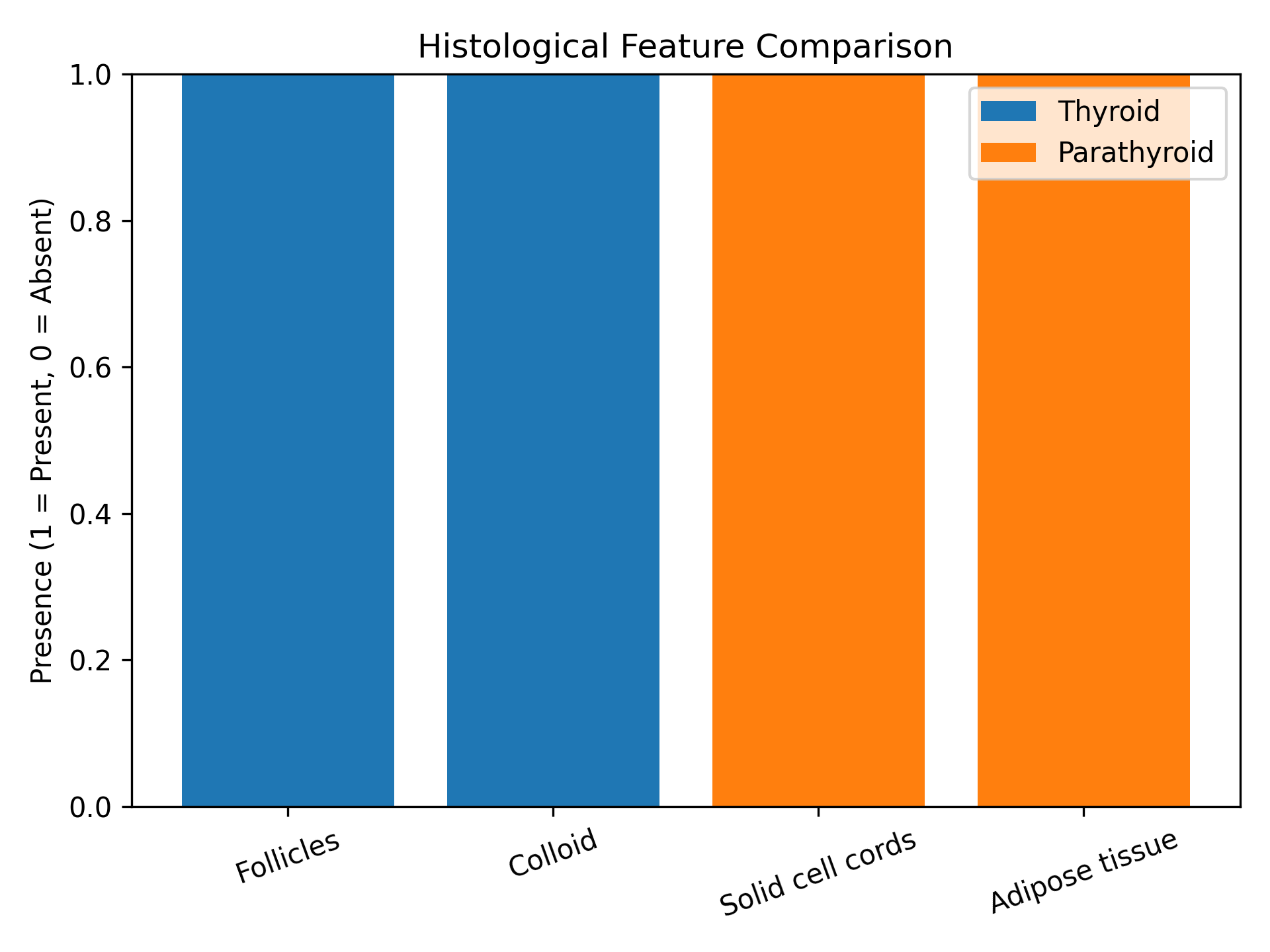
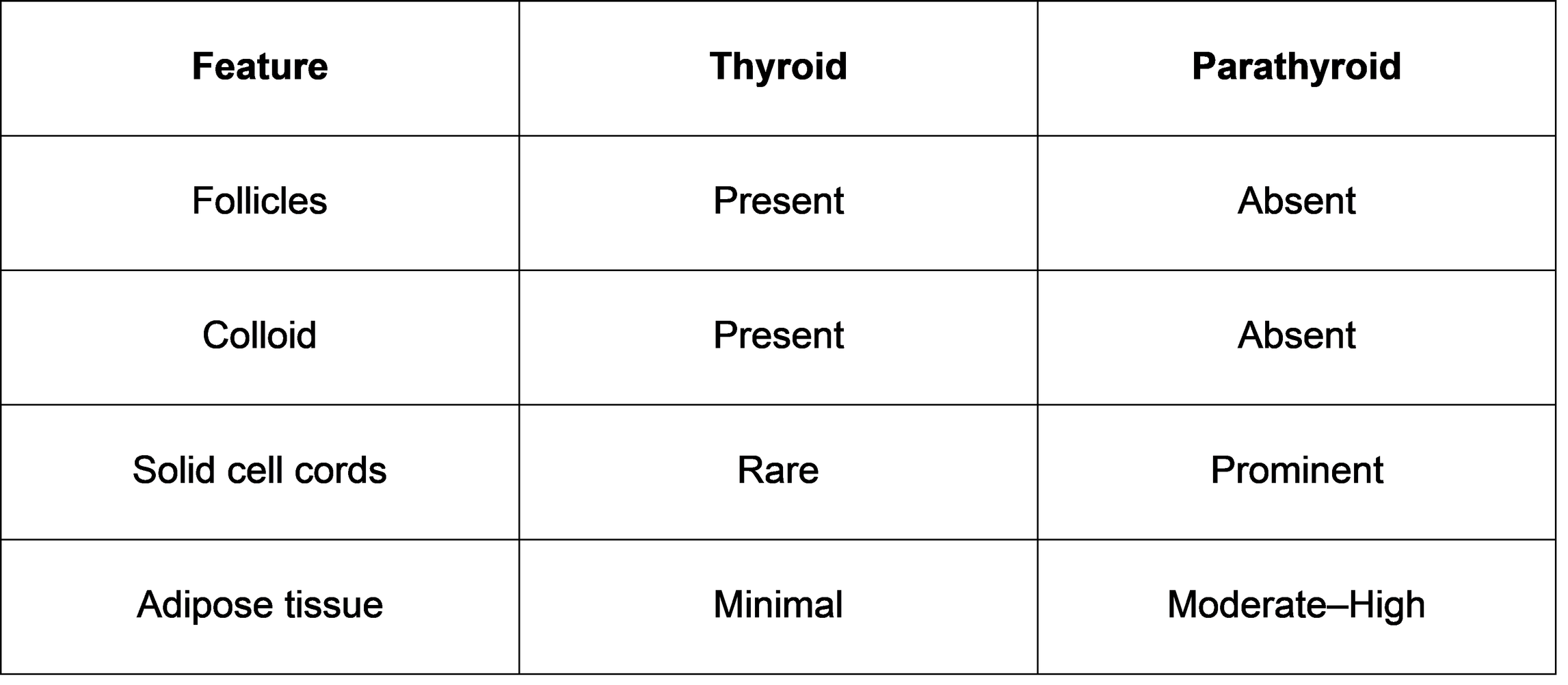
The thyroid gland is enclosed by a thin connective tissue capsule that sends septa into the parenchyma, dividing it into lobules. Each lobule contains numerous spherical thyroid follicles, the functional units of the gland.
Follicular Structure
Each follicle consists of:
● A single layer of follicular epithelial cells
● A central lumen filled with colloid, rich in thyroglobulin
The height of follicular cells varies with functional activity, appearing squamous in inactive states and columnar during active hormone synthesis.
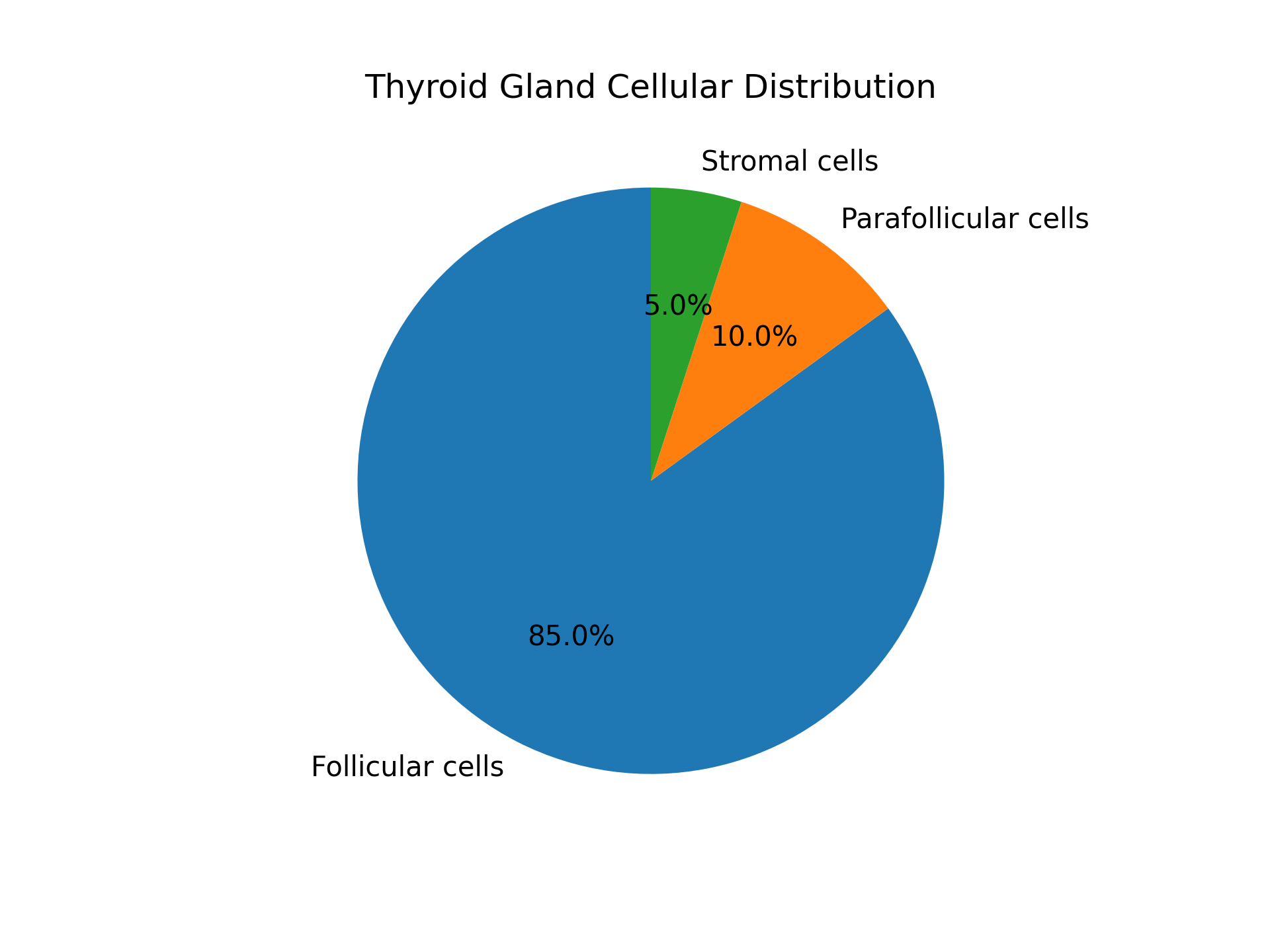
Cell Types
● Follicular cells: Responsible for synthesis, storage, and secretion of T3 and T4
● Parafollicular (C) cells: Located between follicles; secrete calcitonin
Vascularity
The thyroid is highly vascularized, facilitating rapid hormone release into circulation.
Histological Overview of the Parathyroid Gland
The parathyroid glands lack follicular organization and instead display a solid, cord-like arrangement of cells surrounded by a delicate reticular connective tissue framework.
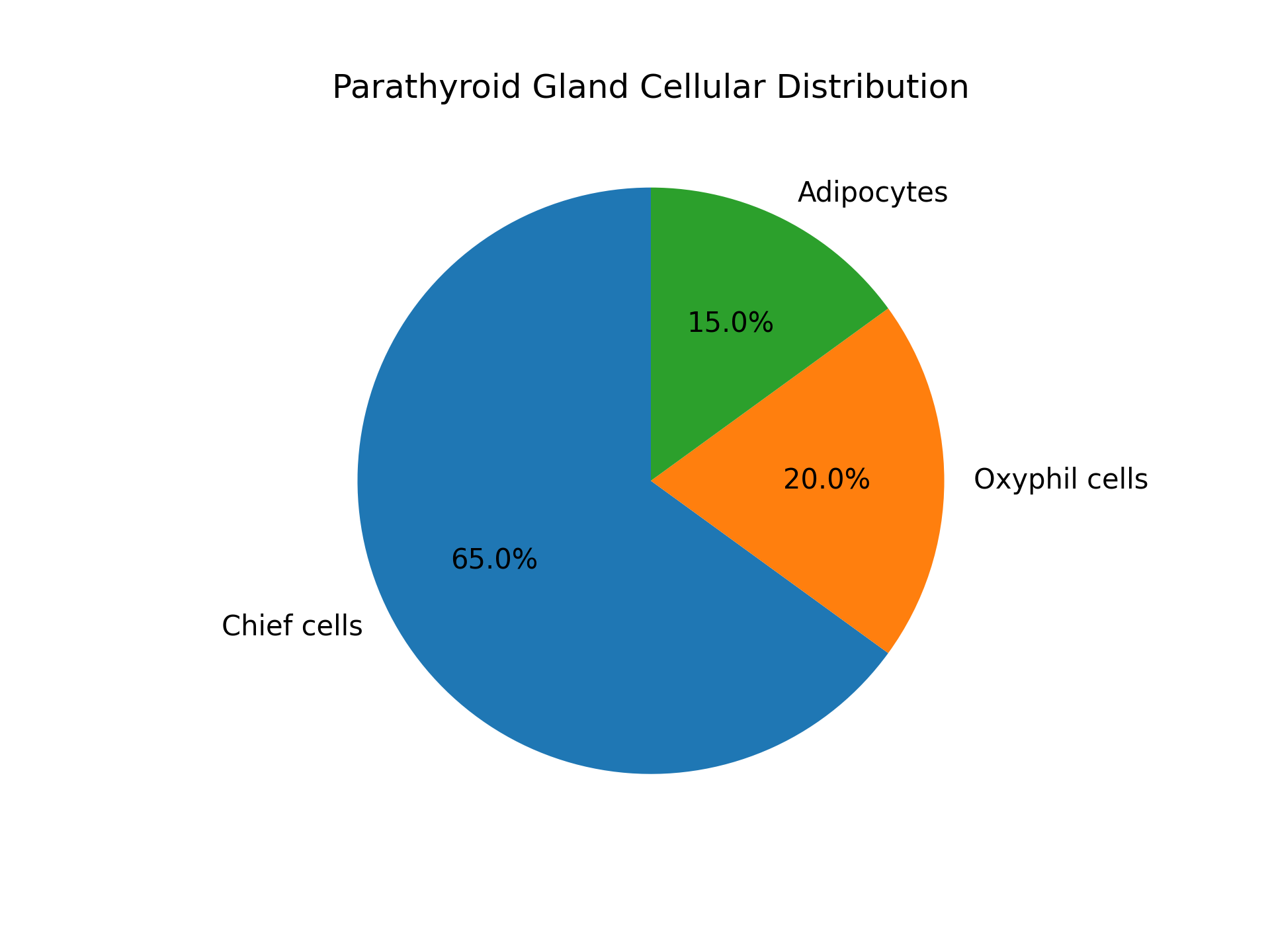
Cell Types
● Chief cells: Small, basophilic cells with central nuclei; secrete parathyroid hormone
● Oxyphil cells: Larger, eosinophilic cells with abundant mitochondria; function remains partially understood
Adipose Tissue
With increasing age, adipocytes infiltrate the parathyroid stroma, sometimes comprising up to 40% of gland volume in adults.
Results
Cellular Composition (Histology-Based)
Pie Chart 1: Thyroid Gland Cellular Distribution (Normal Adult)
Pie Chart 2: Parathyroid Gland Cellular Distribution
Comparative Graph: Structural Organization
Discussion
Histological differences between the thyroid and parathyroid glands are fundamental to their distinct physiological roles. The follicular architecture of the thyroid allows extracellular storage of hormone precursors, a unique feature among endocrine glands. In contrast, the parathyroid gland relies on rapid intracellular hormone synthesis and release, reflected in its solid cellular organization.
The presence of parafollicular cells within the thyroid highlights its minor role in calcium regulation, whereas the dominance of chief cells in the parathyroid underscores its primary function in calcium homeostasis. Age-related adipose infiltration of the parathyroid gland is a key histological marker used to differentiate normal from hyperplastic tissue.
Strengths
● Purely histology-based approach
● Clear structure–function correlation
Limitations
● Lack of primary microscopic slides
● Descriptive rather than experimental
Conclusion
Histological examination of the thyroid and parathyroid glands reveals distinct structural organizations that directly support their endocrine functions. The thyroid’s follicular architecture facilitates hormone synthesis and storage, while the parathyroid’s solid cellular arrangement enables rapid regulation of calcium metabolism. Recognition of these normal microscopic patterns is essential for accurate diagnosis of endocrine disorders and for effective medical education. Histology remains a cornerstone of endocrine pathology and clinical correlation.
Suggestions / Recommendations
Greater emphasis on comparative histology in medical curricula
Routine histological correlation in endocrine diagnostics
Future studies integrating histology with immunohistochemistry
Development of digital histology atlases for endocrine organs
References
Khan YS, et al. Histology, Thyroid Gland. https://www.ncbi.nlm.nih.gov/books/NBK551659/
Brown MB, et al. Histology, Parathyroid Gland. StatPearls [Internet].
https://www.ncbi.nlm.nih.gov/books/NBK546596/Beynon ME, et al. An Overview of the Thyroid Gland and Thyroid-Related Histology.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6507001/Das SS, et al. Development of Parafollicular Cells and Their Relationship to Thyroid Follicles.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5583831/Arauchi A, et al. Functional Thyroid Follicular Cells Differentiation. Frontiers in Endocrinology (histological aspects). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5439004/
Kim S, et al. The Parathyroid Gland: An Overall Review of the Hidden Endocrine Organ.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11009140/TeachMePhysiology.com – Thyroid & Parathyroid Gland Structure and Function (histology diagrams + descriptions). https://teachmephysiology.com/endocrine-system/thyroid-parathyroid-gland/
SEER Training Modules – Thyroid & Parathyroid Glands Anatomy & Microscopy (educational resource). https://training.seer.cancer.gov/anatomy/endocrine/glands/thyroid.html